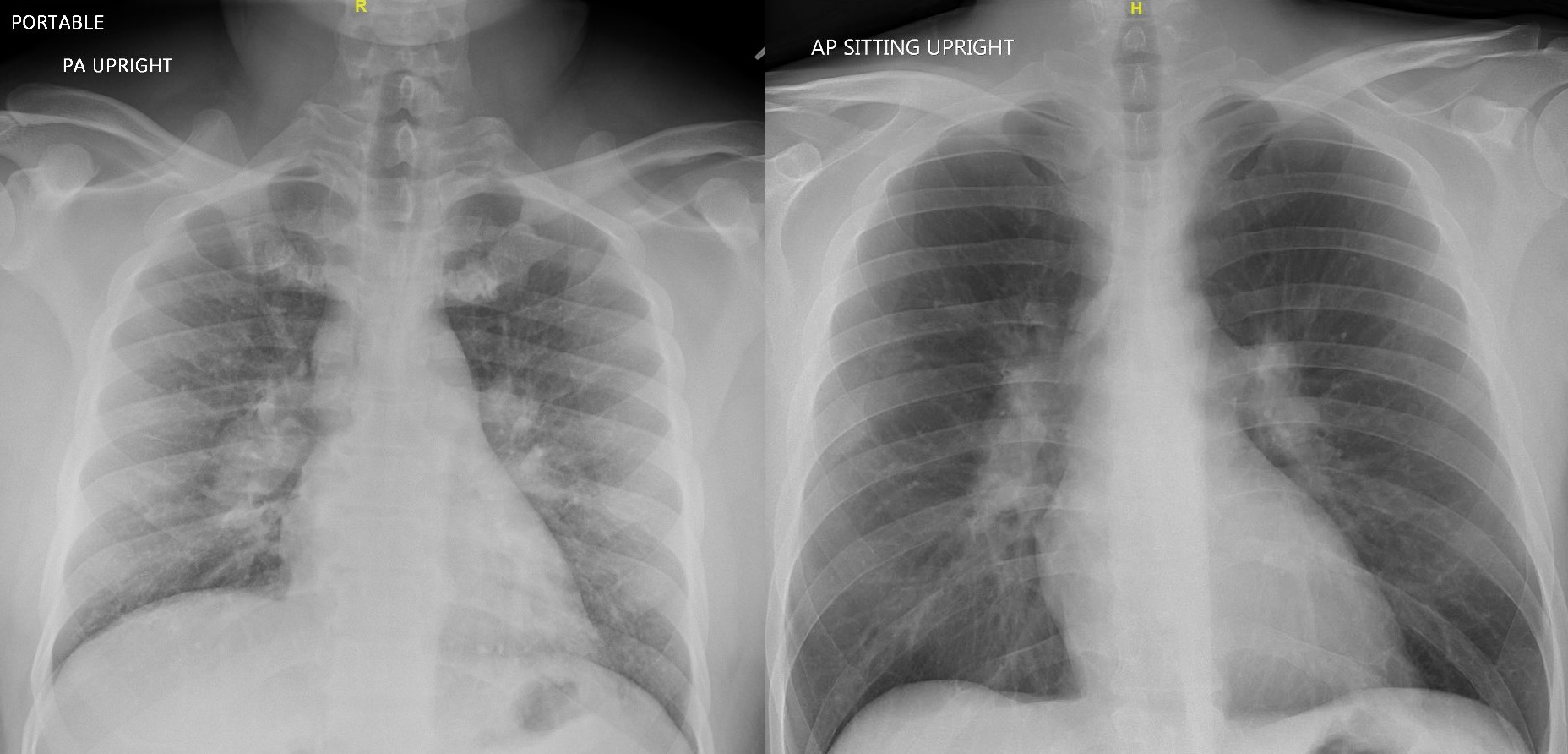
Case Presentation: Case 1A 49 year old male without past medical history presented to the hospital with 2 weeks of painful bilateral ankle swelling followed by chest pain, cough, and fever. He denied family history of autoimmune disease. Chem 7 and complete blood count were unremarkable. Lower extremity ultrasonography was negative for deep venous thrombosis. Antibiotics were started given initial suspicion for cellulitis. These were discontinued once chest x-ray revealed bilateral hilar adenopathy consistent with sarcoidosis. Follow-up chest CT confirmed extensive hilar and mediastinal adenopathy with scattered pulmonary nodules. Serum angiotensin converting enzyme (ACE) was high at 111 U/L. Interferon gamma release assay (IGRA) was negative. The patient’s presentation was highly specific for Löfgren syndrome (LS), an acute form of sarcoidosis. Naproxen was initiated and he was discharged with outpatient pulmonology followup.Case 2A 35 year old male with no past medical history was admitted with 1 week of fevers; severe bilateral hand, wrist, knee, and ankle pain; and a painful nodular rash over his arms and legs. He had recently been treated with outpatient amoxicillin for presumed cellulitis without improvement. He denied respiratory or GI symptoms. Family history was negative for autoimmune disease. Workup was notable for C reactive protein 148.84 mg/L, erythrocyte sedimentation rate 40 mm/h, and bilateral hilar and mediastinal lymphadenopathy on chest imaging. Infectious workup including IGRA was unremarkable. A punch biopsy of his rash demonstrated erythema nodosum, supporting a diagnosis of LS.Given the severity of his symptoms and lack of improvement with first line nonsteroidal anti-inflammatory drugs (NSAIDs), prednisone was initiated with dramatic clinical improvement. He was discharged on hospital day 2 with a prednisone taper and rheumatology follow up.
Discussion: LS is a prognostically favorable form of acute sarcoidosis characterized by fever, erythema nodosum, hilar adenopathy, and symmetrical polyarthritis, involving the ankles in >90% of cases. Median age of presentation is 30-40. Symptoms are often self-limiting, with 81% of patients in spontaneous remission at 2 years in one cohort. HLA-B8/DR3 is strongly associated with the disease, and may predispose towards T helper 1 and macrophage overactivation. LS may mimic cellulitis and infectious arthropathy. Patients often present to inpatient settings for evaluation when they do not respond to outpatient antibiotic therapy. Unlike many other rheumatologic conditions, LS does not require a histologic diagnosis; the presence of the above clinical and imaging findings has 95% diagnostic specificity. Prompt recognition of its pathognomonic features can spare LS patients from prolonged hospital stays and costly invasive workup. Most patients respond well to NSAID monotherapy. A prednisone taper may be used for those with severe refractory symptoms. Ophthalmology referral should be considered to screen for associated uveitis.
Conclusions: LS should be suspected in patients presenting with acute-onset fever, polyarthritis involving the ankles, and erythema nodosum, with hilar adenopathy on imaging. Diagnosis does not require biopsy, though pulmonary tuberculosis must be ruled out. The clinical course is frequently benign. Patients may be treated supportively with NSAIDs and discharged with pulmonology or rheumatology follow up to ensure disease resolution.