Background: The after-visit-summary (AVS) is an essential tool used by providers to explain discharge instructions and ensure appropriate post discharge follow up. Studies have shown that post discharge follow up within 7 days is associated with substantially lower risk of readmission, an organizational priority for us (1). However, many patients were not following up within that time frame. Additionally, the current AVS was time consuming, repetitive, and lacked clarity for both providers and patients. Our goal was to improve the provider experience with the AVS and improve post discharge follow up at our institution at 7 days for patients.
Methods: A multidisciplinary team, composed of case management, nursing, pharmacy, hospitalists, and information technology (IT), collaborated to redesign the AVS for 4 hospitals. The project took place over 5 phases (table 1), with each specialty contributing strategies for improvement. The AVS was also taken to the Patient and Family Advisory Council (PFAC) for feedback, ensuring that our redesign incorporated the patients’ perspectives as well. We then compared pre and post surveys of providers to see how their experience with the AVS redesign was, and we followed trends for post hospital follow up at 7 and 14 days.
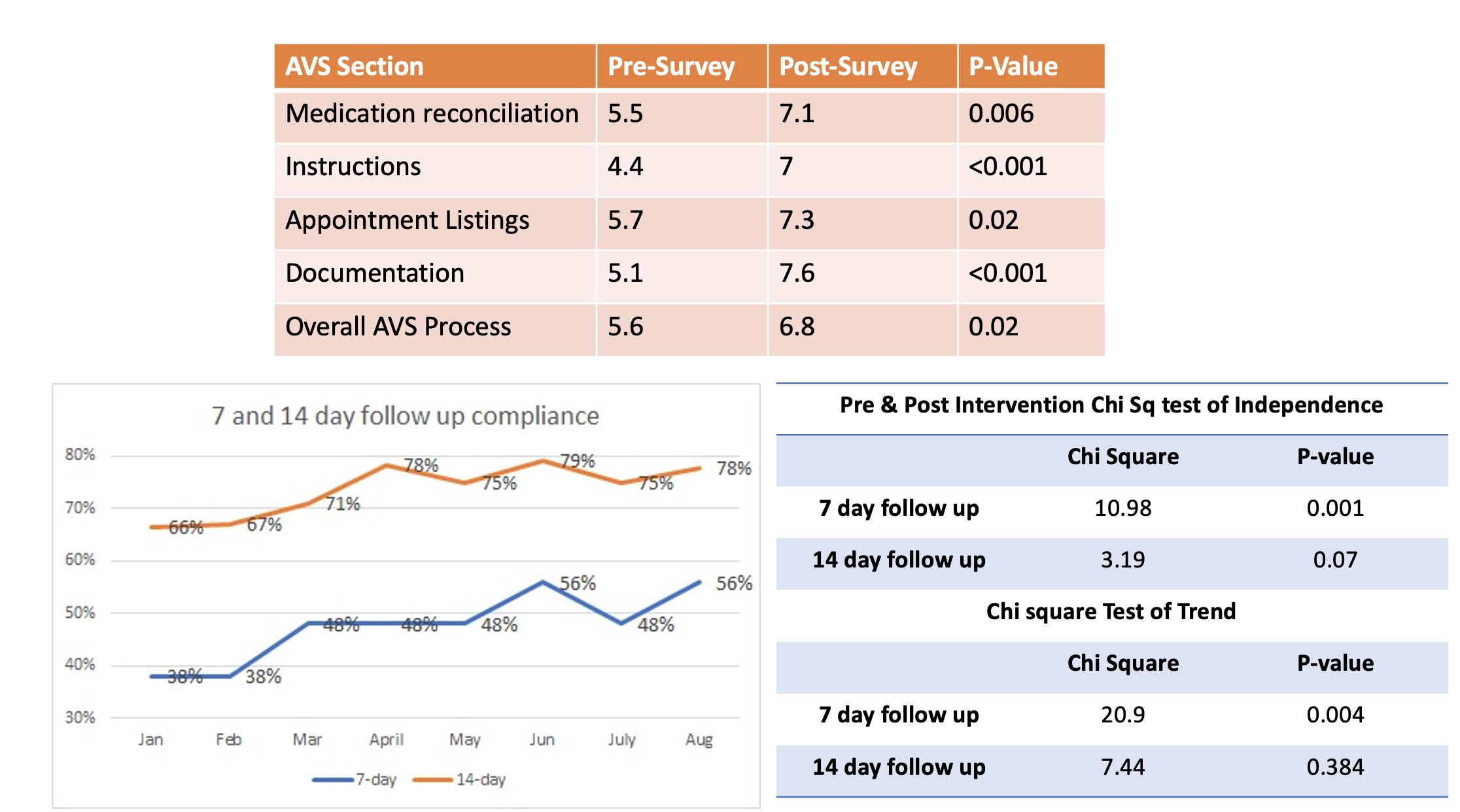
Results: Post-redesign surveys completed by providers showed statistically significant improvements in all facets of the AVS. Using a paired sample two tailed test of means, we compared mean survey scores in the pre and post surveys in these 5 domains: medication reconciliation (Pre-Mean 5.5, Post-Mean 7.1, P-value 0.006), clarity of discharge instructions (4.4 vs 7, P-value < 0.001), appointment scheduling (5.7 vs 7.3, P-value 0.02), documentation ( 5.1 vs 7.6, P-value < 0.001), and the overall AVS process (5.6 vs 6.8, P-value 0.02) (figure 2).To examine the impact of post discharge 7 day and 14 day follow up, we examined data from two distinct periods: January to April (pre-intervention) and May to August (post-intervention). We utilized the chi-square testing to evaluate the differences and trends. For the Chi-square test of independence pre and post intervention for the 7-day follow-up, we observed a significant association (χ² = 10.98, p = 0.001) between the intervention and improved compliance. Similarly, for the 14-day follow-up, while the association was not statistically significant (χ² = 3.19, p = 0.07), there was a notable trend towards improvement. When we examined the chi-square test of trend for the entire period from January to August, we also found improvements in both 7-day (χ² = 20.9, p = 0.004) and 14-day (χ² = 7.44, p = 0.384) follow-up rates (figure 2). The 7-day follow-up rate displayed a particularly significant positive trend, indicating a consistent enhancement over the study period.
Conclusions: A multidisciplinary team approach to AVS redesign can enhance discharge instruction clarity, and subsequently improved post discharge patient follow up within 7 days. AVS redesign can also improve the provider experience. Further data is being collected to see impact on readmission rates.