Background: Despite the importance of sleep to recovery from acute illness and the patient experience, hospitalizations are far from restful. Currently, Medicare focuses on noise, but other disruptions to patient sleep such as lab draws, vitals and pain must also be considered. In order to improve in-hospital sleep via a patient-centered approach, it is important to understand how patients, physicians and nurses perceive potential sleep disruptions and to identify which disruptions are most linked to objective sleep loss.
Methods: Patients and hospital staff completed the Potential Hospital Sleep Disruptions and Noises Questionnaire (PHSDNQ). Cut points were defined based on means, and responses were dichotomized. Perceived percent disrupted for each item was calculated, and responses were compared across groups using chi-squared tests. The association between patient reported disruptions and objective sleep time was assessed using an actigraphy study, where patients completed the PHSDNQ each day and wore an Actiwatch to record sleep duration. A multivariable linear regression model controlling for subject random effects examined the association between patient-reported disruptions and sleep duration.
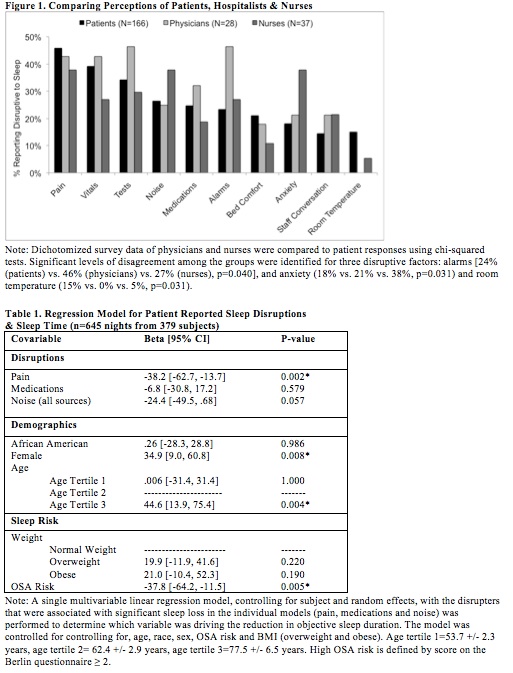
Results: 166 patients, 28 hospitalists (78%) and 37 nurses (88%) completed the PHSDNQ. Patients, hospitalists and nurses agreed that pain, vitals and tests were among the top three disruptive factors to patient sleep. There were significant differences among the groups’ responses for alarms [24% (patients) vs. 46% (hospitalists) vs. 27% (nurses), p<0.040], room temperature (15% vs. 0% vs. 5%, p<0.031) and anxiety (18% vs. 21% vs. 38%, p<0.031). In the multivariable linear regression model including data from 645 nights of 379 patients, pain was the only variable associated with significantly less sleep duration (minutes) [-38.2 (95% CI -62.7, -13.7) p<0.002].
Conclusions: Clinicians generally agreed with patients on what disrupts in-hospital sleep, and all three groups identified pain as a top disrupter. Further, pain was associated with greatest objective sleep loss, highlighting the need for better pain management.