Background: Academic hospitalists have identified teaching learners as the most fulfilling aspect of their jobs. Components of effective clinical education include teaching at the bedside and giving feedback. To enhance and develop the teaching and professional developmental skills of early-career hospitalists, the Society of Hospital Medicine (SHM), the Society of General Internal Medicine (SGIM), and the Association of Chiefs and Leaders of General Internal Medicine (ACLGIM) created the Academic Hospitalist Academy (AHA), an annual conference of lectures and workshops. Our study aims to identify the barriers to teaching effectively at the bedside and providing feedback to learners as identified by academic hospitalists attending AHA.
Methods: As part of AHA enrollment, all attendees are asked to complete an anonymized, voluntary survey prior to the start of the conference. The survey includes questions about participant demographics, barriers to teaching at the bedside, and barriers to providing feedback to learners. We collected the survey responses from all 11 years of the AHA (2009 to 2019) and coded and categorized the free-response answers.
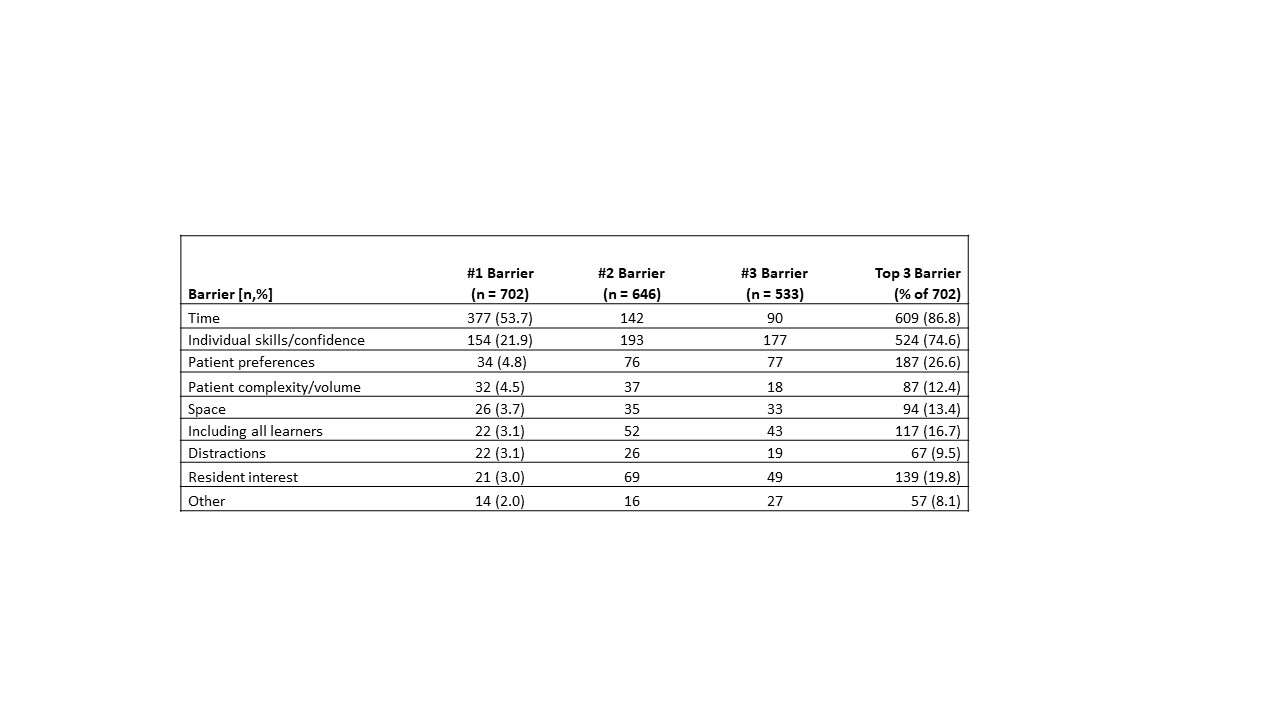
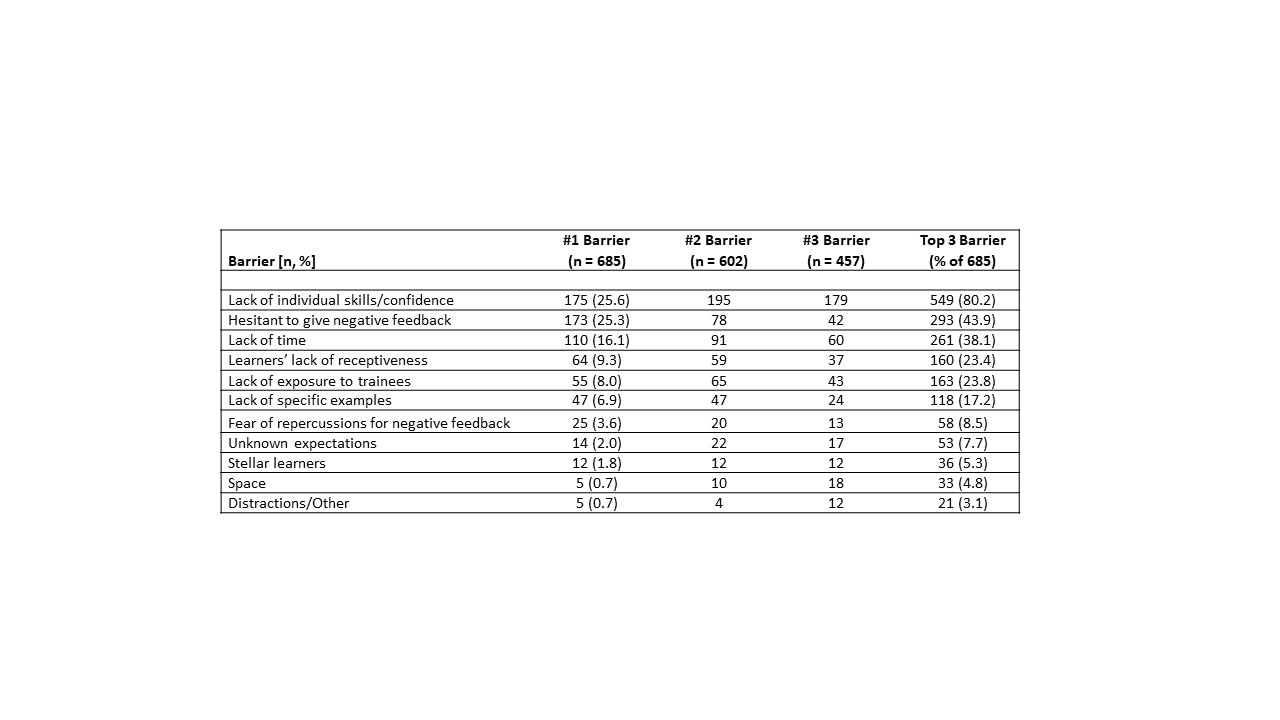
Results: The average age of AHA attendees was 34 years, and attendees have an average 3.2 years of hospitalist experience. Of the 812 hospitalists who completed the survey, 702 (86.4%) identified barriers to bedside teaching and 685 (84.4%) identified barriers to providing feedback. Lack of time was the most commonly reported barrier to bedside teaching, reported by 86.8% of hospitalists, and named as the leading barrier by the majority of hospitalists (53.7%). Lack of confidence in bedside teaching skills was also named as a barrier by a majority of hospitalists (74.6%). Barriers to providing feedback included a lack of confidence in individual skills, listed as a barrier by 80.2% of hospitalists, followed by difficulty giving negative feedback (43.9%) and lack of time (38.1%).
Conclusions: Time constraints and lack of confidence in individual skills are the most common barriers to bedside teaching and providing feedback reported by academic hospitalists. With these data, AHA and other groups engaged in hospitalist career development and clinical education can better tailor their training to the needs of academic hospitalists.