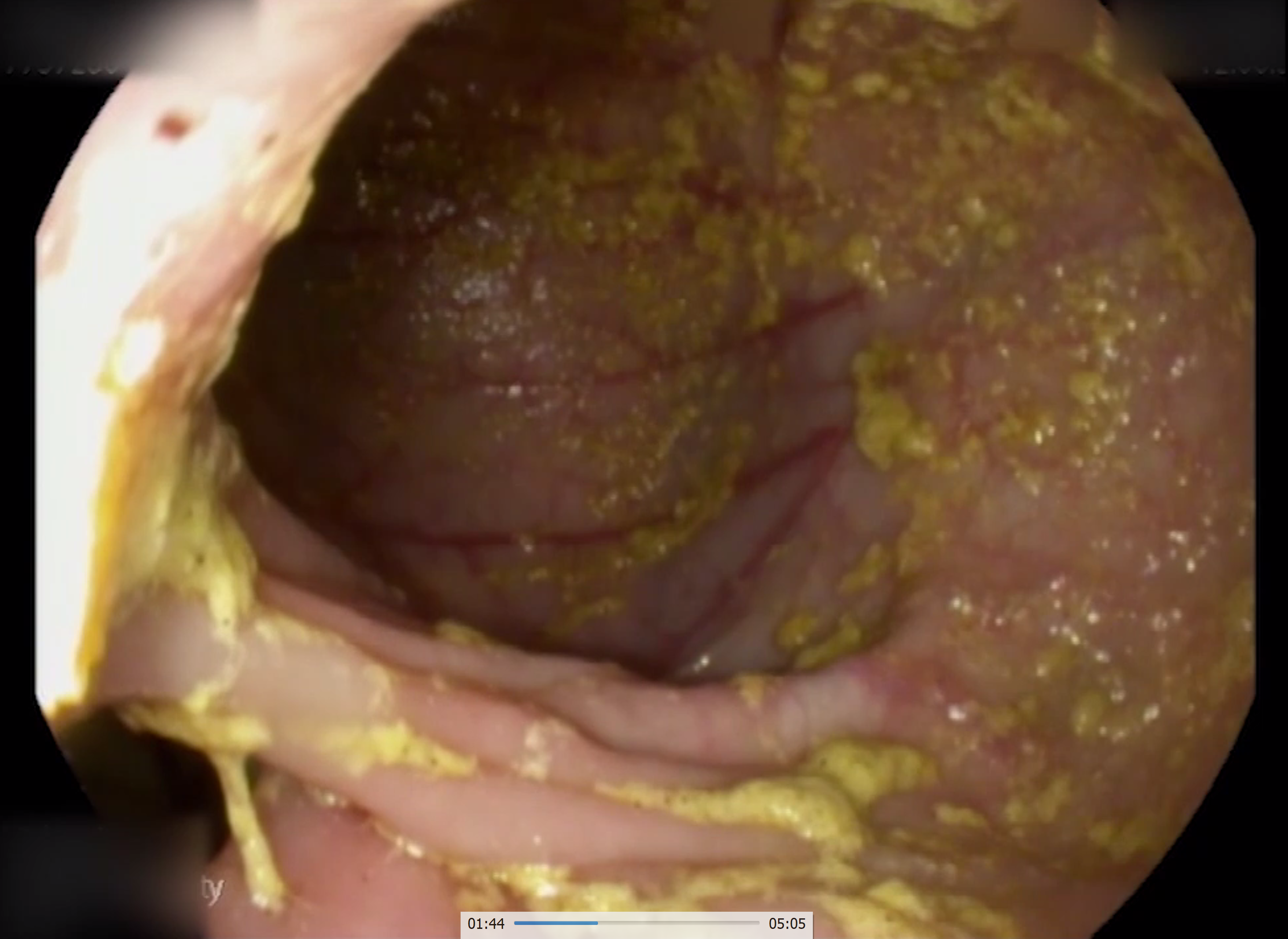
Case Presentation: The patient is a 61-year-old male theatre director who presented with chronic diarrhea associated with a 50-pound weight loss, fatigue, and weakness. His past surgical history was notable of a Whipple’s procedure done 10 years ago for a symptomatic duodenal mass causing nausea and vomiting, later found to be benign in nature. Patient reported that he had been having profuse watery diarrhea multiple times a day for the last one year. A trial of lactose-free diet and a course of antibiotics did not improve his symptoms. Upon further investigations, it was revealed that the patient had anemia, hypokalemia and a low albumin level. Workup was negative for celiac disease, carcinoid syndrome, gastrinomas, etc and therefore the patient had an endoscopy which revealed a benign gastro-colic fistula in the setting of an anastomotic pyloric ulcer eroding into the transverse colon (Fig 1, Fig 2). This was confirmed by an abdominal CT scan with contrast and Upper GI series roentgenogram. He was then referred for surgery following optimization of his nutritional status.
Discussion: Gastro-colic fistulas were first described as a complication of gastric cancer in 1755 by Albrecht von Haller. A majority of cases are due to malignancy, specifically gastric cancer or transverse colon cancer, although fistulas due to benign causes have also been described. In addition, cases of gastro-colic fistula have been observed in the setting of prior gastric surgeries but the interval duration of development has been reported to be around 8 to 9 months. Patients generally present with undifferentiated symptoms like diarrhea, weight loss, abdominal pain, nausea and vomiting making the diagnosis difficult. Radiologic imaging studies such as barium enema (most sensitive test) and barium meals are the mainstay of diagnosis. Endoscopy is usually not recommended as a diagnostic tool as the fistula may be missed in between the gastric folds. Endoscopy with biopsy is primarily done as part of the workup to rule out malignancy. Definitive treatment includes surgical en-bloc resection. Conservative medical management such as proton pump inhibitors with or without fibrin sealant should be considered when surgery is contraindicated or in those cases that occur in the setting of peptic ulcer disease. Our patient had a perforating peptic ulcer at the gastro-jejunostomy anastomotic site that was able to create a fistula to the colon due to distorted post-surgical anatomy.
Conclusions: This case highlights the importance of considering structural abnormalities as a cause of chronic diarrhea, especially in patients with prior abdominal surgery even if it presents as late as 10 years post surgery.