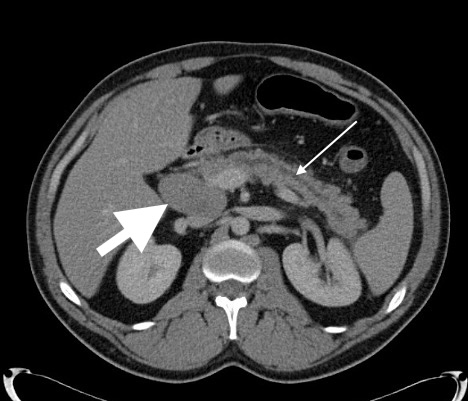
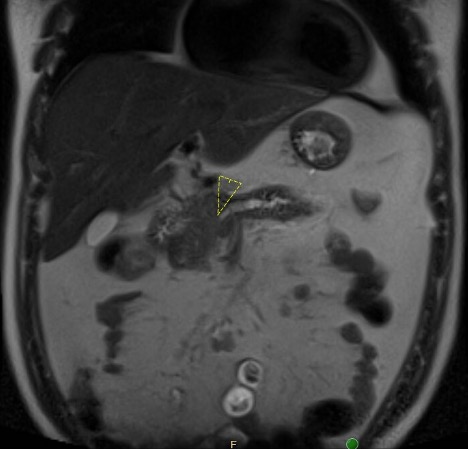
Case Presentation: A 29-year-old male with no medical history presented with abdominal pain and diarrhea after a trip to Key West. He described 2 days of constant epigastric pressure and cramping with no relation to food intake or bowel movements, along with 1 night of black, watery diarrhea. He denied fever, weight loss, night sweats, or easy bleeding/bruising. He endorsed daily binge drinking while traveling, with no consumption of raw shellfish, illicit drug use, or unprotected sexual encounters. He lived in rural North Carolina and owned dogs, chickens, and cats. He had a 5 pack year smoking history and used no medications. Family history was significant for a “lymph node cancer” in his father. At presentation, vital signs were T 37.1°C, HR 96 bpm, BP 185/100 mmHg, RR 18, and SpO2 96% on room air. Exam showed epigastric tenderness with no cervical lymphadenopathy or jaundice. Laboratory results showed WBC 11.7 x10*9/L (H), Hgb 12.7 g/dL, Platelets 371 x10*9/L, absolute neutrophil count 9.2 x10*9/L (H), and absolute lymphocyte count normal. Elevated studies included fibrinogen 585 mg/dL, lipase 1,100 U/L, CRP 30 mg/L, and ESR 30 mm/h. Notably normal studies included a complete metabolic panel, lactate, APTT, PT, INR, GI stool pathogen panel, C. difficile assay, and ova/parasite exam. Peripheral smear showed a mild normocytic anemia. CT abdomen/pelvis showed acute interstitial pancreatitis, dilation of the main pancreatic duct, and multistation adenopathy throughout the abdomen and pelvis. A magnetic resonance cholangiopancreatography (MRCP) showed multifocal abnormal soft tissue deposits within the pancreas obstructing the main pancreatic duct. Both studies suggested a concern for lymphoma. Malignant hematology was initially unimpressed with his case due to the near normal CBC and normal LDH and uric acid. As such, an infectious workup for diffuse lymphadenopathy was pursued and negative for HIV, syphilis, tuberculosis, tick-borne illnesses, bartonellosis, and toxoplasmosis. He underwent EUS/ERCP with main pancreatic duct stenting and biopsy. Pathology ultimately resulted as diffuse large B-cell lymphoma.
Discussion: Acute pancreatitis is a common inpatient diagnosis, most frequently caused by gallstones and alcohol use. Lymphoma, as described in our case, is an exceedingly rare cause of acute pancreatitis. Pancreatic lymphoma is rare, accounting for less than 0.5-1% of all pancreatic malignancies (1). Non-Hodgkin’s lymphoma is commonly associated with extra-nodal extramedullary involvement; however, only 0.2-2% of patients have pancreatic involvement at diagnosis (1,2), most commonly seen with diffuse large B-cell lymphoma. Patients with pancreatic lymphoma can present with classic pancreatitis symptoms, but less commonly have associated constitutional symptoms that are typical of non-Hodgkin’s lymphoma, making diagnosis more difficult. Prompt identification of pancreatic lymphoma is important, as it is usually responsive to standard chemotherapy (2,3).
Conclusions: Acute pancreatitis is a common inpatient diagnosis with increasing prevalence, and a broad differential should be considered, especially when presentation is not classic. Pancreatic lymphoma, specifically extra-nodal non-Hodgkin’s lymphoma, is a rare and difficult to diagnose etiology of pancreatitis. Thus, it is important for hospitalists to have a high index of suspicion, especially when initial history and work up are non-specific.