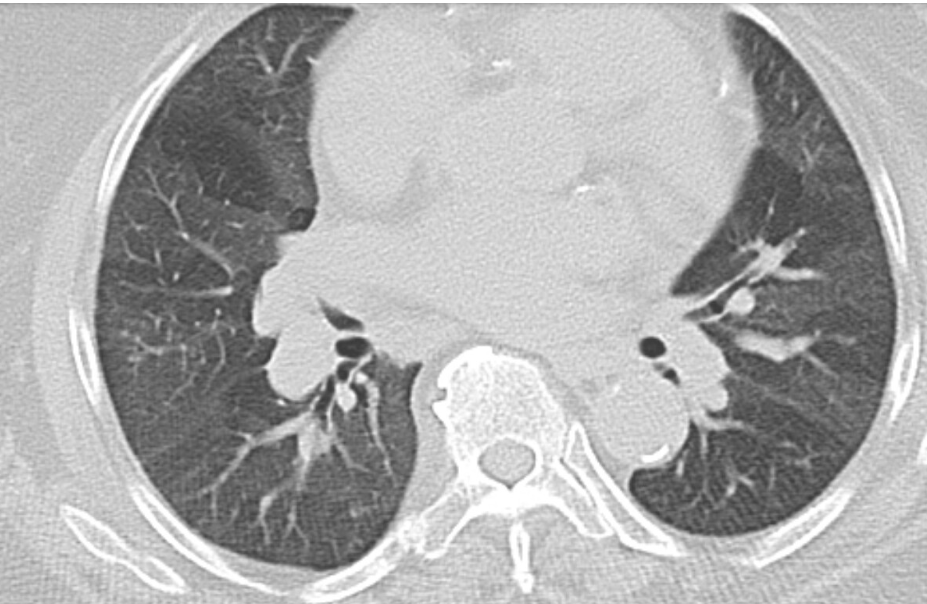
Case Presentation: Clinical presentation: A 69-year-old female presented to the emergency for shortness of breath and bilateral low extremity edema. She had a history of chronic dyspnea and hypoxia on baseline 2 liters of oxygen and reported worsening dyspnea on minimal exertion for the week prior to admission. Review of symptoms was significant for wheezing episodes, arthralgia in bilateral hands and knees, and low extremities and lower back muscle skeletal pain. She had a documented history of chronic obstructive lung disease (COPD) on baseline 2 L of oxygen, pulmonary hypertension, type 2 diabetes, atrial fibrillation, and heart failure with preserved ejection fraction (HFpEF). No smoking history, alcohol, or drug abuse. On admission the working diagnosis was a COPD versus HFpEF exacerbation. She received IV furosemide, prednisone, and azithromycin. After a week of treatment for COPD exacerbation and diuresis, the patient still had dyspnea with minimal exertion. On further review of her history, the patient did not undergo pulmonary function testing, and the diagnosis of COPD was made based on wheezing and a history of second-hand smoke exposure from her spouse. At this point considering the lack of objective evidence of COPD, further work up was pursued to elucidate the acute on chronic dyspnea. Chest tomography showed diffuse mosaic attenuation corresponding with areas of air trapping, mild tree-in-bud nodularity in right middle lobe and an indeterminate 5mm nodule in the right lower lobe. Hand radiograph showed erosions and polyarticular joint space narrowing in the metacarpophalangeal joints and intercarpal joints suggestive of inflammatory arthritis. Laboratory work up showed negative ANCA, dsDNA and ENA, C3 134mg/dL, C4 35.2 mg/dL, CRP 73.7mg/L, RF 269 IUnits/ml, ESR 68mm/hr, ANA 1:320, and CCP Ab >300units/mL. Pulmonary function tests were suggestive of restriction with no obstruction. The patient was diagnosed with seropositive erosive rheumatoid arthritis (RA) and bronchiolitis obliterans (BO). The patient was started on azithromycin and plans to follow up as outpatient to start azathioprine.
Discussion: This patient was misdiagnosed with COPD which led to delay of rheumatoid arthritis and bronchiolitis treatment for 5 years. This case is important to hospitalists as it illustrates situations where misdiagnoses are carried forward in the medical chart. COPD diagnosis requires appropriate clinical context (most commonly smoking history), clinical syndrome and PFTs.1 Only 18% to 69% of patients with physician-diagnosed COPD undergo spirometry.2 BO is another obstructive disease caused by destruction of bronchiolar epithelium. The connective-tissue disease most often associated with it is RA.3 Mosaic-attenuation is the most common radiographic finding of BO at diagnosis. 4
Conclusions: This is a case of a physician-misdiagnosis of COPD with no smoking history nor PFTs. Diagnostic reconciliation and treatment failure prompted further work-up which revealed a new diagnosis. This case illustrates the potential harms of carrying forward inaccurate data in the EMR and the importance of following diagnostic criteria.