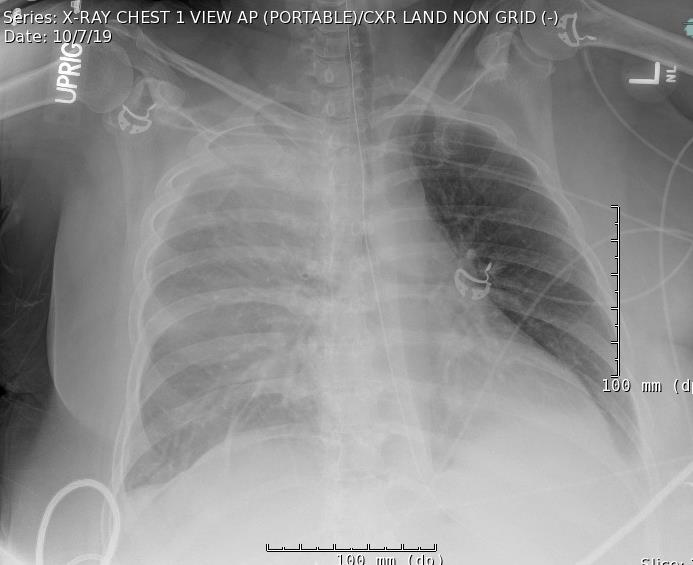
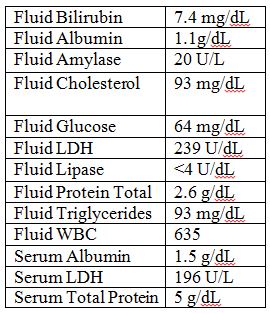
Case Presentation: The patient is a 51 year old female with a history of acute cholecystitis status post cholecystectomy who presented to the hospital for acute on chronic abdominal pain. Since her cholecystectomy five months prior, she had recurrent episodes of nausea, vomiting, and abdominal pain with persistently elevated LFTs and bilirubin. Liver biopsy and ERCP were consistent with sclerosing cholangitis, and a biliary stent was placed. She was later readmitted due to stent malpositioning and had a percutaneous transhepatic biliary drain (PTBD) placed ten days after her initial stent placement; she clinically improved and was discharged home. One week after discharge, she returned for abdominal pain, back pain, and dyspnea. She was afebrile and hemodynamically stable. Labs were remarkable for alkaline phosphatase 253, ALT 21, AST 63, total bilirubin 7.5, white blood cell count of 6.4K, and hemoglobin 10.7. CT scan of abdomen/pelvis with contrast showed a properly positioned biliary drain, small amount of fluid in the falciform ligament, and bilateral pleural effusions. Her chest x-ray showed bilateral pleural effusions, worse on right (see figure 1). Right sided thoracentesis was performed with removal of 1 liter of green fluid and subsequent improvement in pain. Pleural fluid studies were exudative in characteristic and notable for bilirubin of 7.4 mg/dL, consistent with bilothorax (see figure 2). She was treated with ceftriaxone and metronidazole for seven days for bile pleuritis. The pleural effusions were concerning for a biliary pleural fistula secondary to the PTBD. The patient underwent cholangiogram demonstrating patent common bile duct draining into duodenum and the PTBD was removed. Her dyspnea resolved and her abdominal pain improved. She did not have recurrence of her pleural effusion.
Discussion: The occurrence of bilious pleural effusion, termed bilothorax, is a rare type of exudative pleural effusion. It is most commonly seen as an isolated right sided pleural effusion, and case reports describing etiologies range from sequelae of liver transplant1, direct biliary-pleural fistula formation from biliary stent migration2, biliary manipulation with subsequent biliary peritonitis and pleuritis3,4, and more. Bile leakage into the pleural space is a dangerous complication that requires prompt recognition, as bile salts can cause severe inflammation in the pleural space leading to pleuritis as well as infection. Our patient developed bilateral bilious pleural effusions after PTBD placement.
Conclusions: Percutaneous biliary drain placement is a fairly common procedure. Common complications of PTBD are bleeding and tube dislocation7. In general, the safety profile of PTBD is not benign; it is known to have more complications than ERCP or endoscopic ultrasound-guided biliary drainage5 for malignant obstruction. Bilothorax, although rare in its occurrence, does occur after PTBD placement as shown in this case. It can occur without the development of a biliary-pleural fistula. Thus, bilothorax should be considered for a patient with recent biliary tree manipulation who develops abdominal pain and/or dyspnea. It is a serious and life threatening condition, as bile salts can cause chemical pleurodesis as well as infection8 and has even been shown to progress to ARDS and death3. Timely recognition of symptoms, clinical investigation with imaging, and treatment with thoracentesis and possible removal of PTBD are essential for avoiding further complications of bilothorax.