Background: The knowledge regarding the association between increased blood pressure variability (BPV) and risk of subsequent clinical outcomes following acute ischemic stroke is not entirely clear. We constructed a cohort of patients hospitalized for new AIS to examine the effect of systolic BPV (SBPV) on the risk of dependency at discharge and 1 year readmission and mortality after the index hospitalization. Further, we conducted a systematic review and meta-analysis to place the current findings in the clinical context.
Methods: Consecutive patients who survived initial hospitalizations for first AIS with a minimum 1-year follow-up were identified from the Mayo Clinic inpatient data base from 2003 to 2019. SBPV was measured as quartiles of standard deviation (SD) from 6 readings obtained during index hospitalization. Outcomes were the development of dependency (modified Rankin Scale [mRS] score ≥ 3) at discharge and readmission and mortality at 1 year following AIS. Electronic data bases were searched for published clinical trials through May 1, 2020, with continued surveillance until November 15, 2020; two investigators independently extracted data, ascertained risks of bias, and graded the strength of evidence. We planned for random-effects meta-analysis to estimate relative risks.
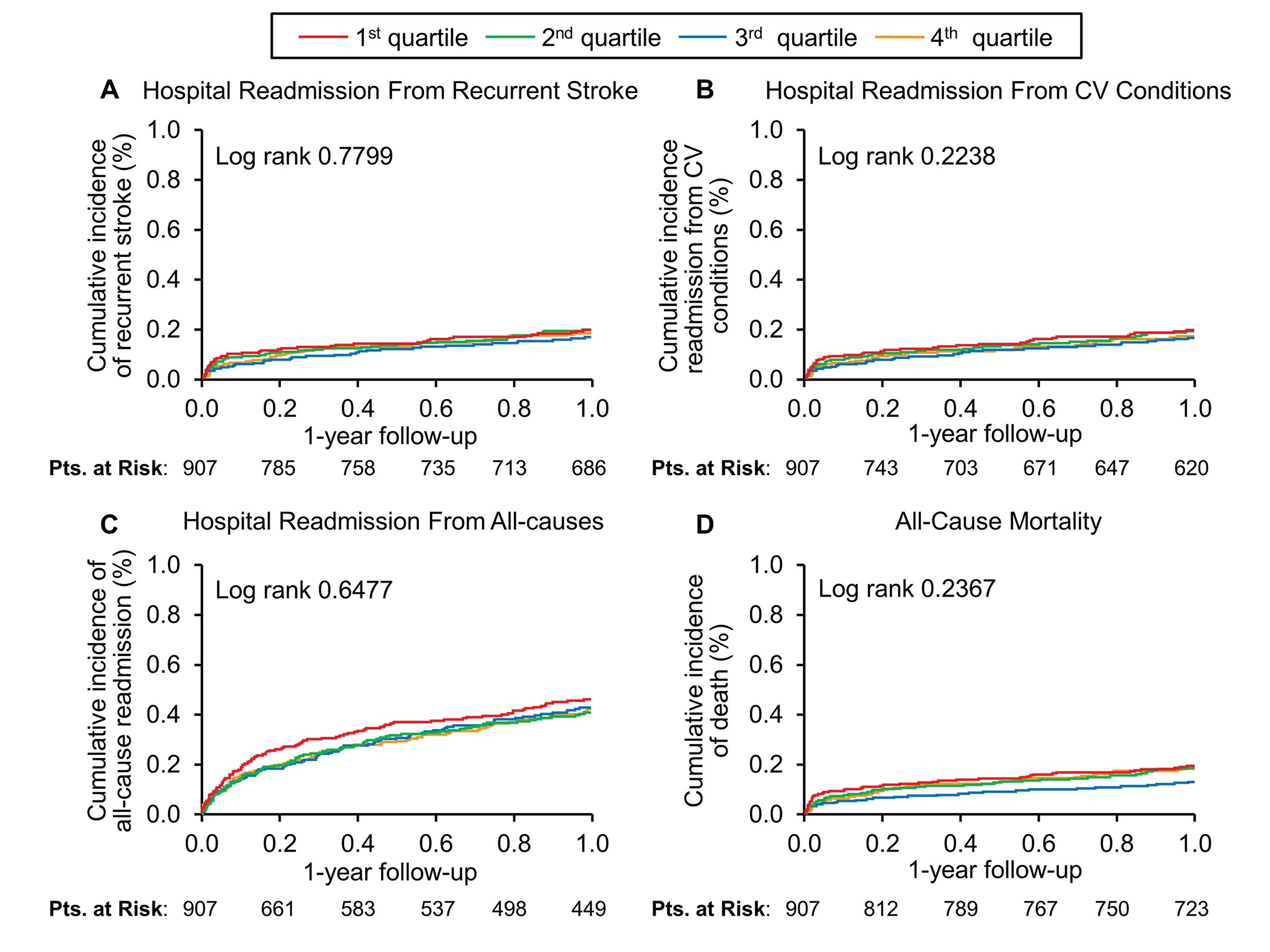
Results: Of 908 AIS survivors, 499 patients (55%) developed dependency at hospital discharge. At 1-year, 354 patients (40%) were readmitted (129 [14%] for cardiovascular causes and 50 [6%] for recurrent strokes), and 162 (18%) patients died. Multivariable logistic and Cox regression models demonstrated that higher SBPV did not predict subsequent dependency (odds ratio 1.00, 95% CI 0.64-1.57) or 1-year recurrent stroke (hazard ratio [HR] 0.96, 95% confidence interval [CI] 0.79-1.16), cardiovascular readmission (HR 0.56, 95% CI 0.78-1.17), all-cause readmission (HR 0.99, 95% CI 0.76-1.27), or all-cause mortality (HR 0.99, 95% CI 0.81-1.24).
Conclusions: The data from cohort study did not demonstrate a statistically significant association between SBPV during hospitalization and risk of dependency at discharge or rates of 1-year hospitalizations or mortality, a finding consistent across key subgroups of patients. The meta-analysis portion of the study was limited by significant heterogeneity across the included studies that posed interpretive challenges.