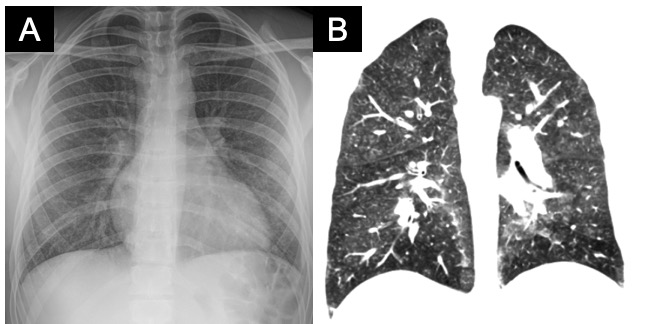
Case Presentation: A 19-year-old man with no medical history presented to gastroenterology clinic with four days of nausea, vomiting, malaise, fevers, and epigastric pain. An esophagogastroduodenoscopy (EGD) was scheduled for the following day. The next morning, the EGD was cancelled when he was found to be to be hypoxemic on pre-procedure vital signs and was sent to the emergency department.In the ED, he was normotensive, febrile to 39.3 C, and tachycardic with a heart rate of 110 bpm. He had a respiratory rate of 20, and his oxygen saturation was 85% on room air. On exam, he had crackles throughout his bilateral lung fields. Complete metabolic panel and complete blood count were unremarkable except for a neutrophilic-predominant leukocytosis to 15.5 k/uL. A comprehensive respiratory viral panel PCR including influenza was sent and returned negative. A CT chest/abdomen/pelvis found no gastrointestinal pathology but did show diffuse centrilobular ground glass and tree-in-bud nodules throughout all lobes of both lungs (Figure). The patient was started on empiric antibiotics for community acquired pneumonia and admitted to the medicine service. Further history revealed no recent travel, animal, nor environmental exposures, but did confirm a two-year history of daily vaping with nicotine, THC, and mint flavored cartridges. He had developed a cough two months prior, which led to cessation of vaping two weeks ago. Pulmonology was consulted for bronchoscopy with bronchoalveolar lavage (BAL). BAL cell count had 1065 nucleated cells with 23% neutrophils, 26% lymphocytes, and 1% eosinophils. BAL samples were negative for fungal, viral, mycobacterial, and bacterial infection. He was initiated on solumedrol 30mg every eight hours for one day then transitioned to prednisone 60mg daily with a plan to taper by 10mg weekly over six weeks. His fevers and GI symptoms resolved within several days of starting steroids, but at discharge he was still requiring 2L of supplemental oxygen. He was seen in pulmonary clinic three weeks later with resolution of his respiratory symptoms and hypoxemia.
Discussion: E-cigarette or Vaping-Associated Lung Injury (EVALI) has a heterogeneous range of symptoms and severity, with some cases resulting in intubation and death[1]. While almost all patients have respiratory symptoms (98%) and constitutional symptoms (99%), gastrointestinal symptoms are nearly as frequent, appearing in 81% of patients: nausea (70%), vomiting (66%), diarrhea (43%), and abdominal pain (43%)2. While diagnostic criteria for vaping-induced lung injury do not yet exist, a proposed case definition for making a clinical diagnosis includes[1,2]: (1)History of e-cigarette or related product use within 90 days, (2)Pulmonary opacities on lung imaging (chest x-ray or CT), (3)Exclusion of infectious causes including negative influenza PCR, viral respiratory panel, (4)Absence of a possible alternative diagnosis[1,2]. Recently, of 29 BAL samples submitted to the CDC, vitamin E acetate(100%) and THC (82%) was found to be highly associated with the lung injury (100%)[4]. The optimal treatment is not established but most cases of treatment have described using steroids with best supportive care.
Conclusions: This case demonstrates how gastrointestinal symptoms presenting as part of EVALI can be misleading. Since the diagnosis is heavily dependent on the physician taking a thorough vaping exposure history, a high-index of suspicion after a thorough smoking history is essential to prompt diagnosis and adequate treatment.