Case Presentation:
A 40‐year‐old blind woman presented with progressively altered mental status 1 week after an emergency department visit for a “viral URI.” PMH was significant for giant optic glioma, anxiety, neurodermatitis, and mild mental retardation.
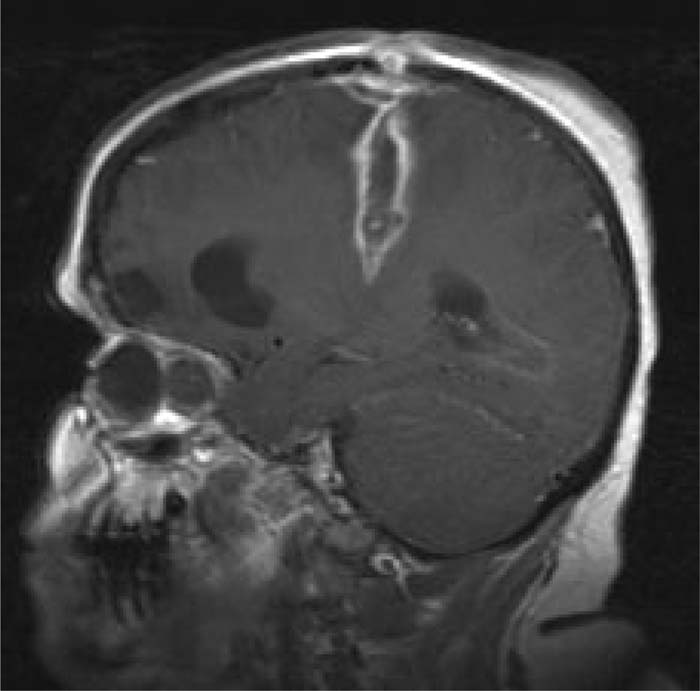
She had a low‐grade fever of 99.3, was awake but nonverbal, and followed only very simple commands. Strength was 1/5 in the right UE and 3/5 in right LE. There was a 2‐cm scabbing lesion on the top of her scalp, reported by her family to be a lesion typical of her neurodermatitis. There were also mild meningeal signs. MRI showed a tracking, ring‐enhancing lesion from the vertex of the skull to the left parietal lobe, consistent with a penetrating trauma. Her family subsequently confessed that 10 days before admission, the patient had admitted probing the lesion on her scalp with a weaving needle “an index finger deep to see how deep it was.”
Empiric vancomycin, metronidazole, and cefepime were initiated along with steroids because of cerebral edema. An emergent craniotomy with abscess drainage was performed. Cultures grew MSSAand fusobacteria. She made an impressive recovery to very near her baseline over 7 days, and was discharged to a rehabilitation facility on a 6‐week course of oxacillin and metronidazole.
Discussion:
Most brain abscesses (40% of cases) originally stem from nasopharyngeal infections. Hematogenous spread accounts for 30% of cases, most commonly from dental infections. Only 10% of cases are the result of direct seeding from trauma or neurosurgical procedures, and the rest are idiopathic. Headache is the most common presenting symptom. MRI is the diagnostic modality of choice because of its ability to distinguish ring‐enhancing lesions from brain neoplasms.
Management includes a combination of IV antibiotics and surgical drainage. Broad‐spectrum empiric antibiotics should be started as soon as possible, with the spectrum narrowed once the pathogen is identified, and continued for 6‐8 weeks, depending on the clinical course. Rapid progression of the infection before hospitalization, severe mental status changes on admission, stupor or coma, and rupture into the ventricle(s) are associated with a poor prognosis. However, recent studies show that both morbidity and mortality have decreased, most likely because of advances in diagnostic modalities, antibiotic regimens, and surgical techniques.
Conclusions:
Hospitalists, among all other physicians in the acute care setting, should be aware that the manifestations of brain abscess initially tend to be nonspecific, resulting in a delay of diagnosis. A high level of suspicion based on a good H & P is probably the most valuable tool for a prompt diagnosis. This, along with empiric broad‐spectrum antibiotics, and neurosurgical intervention, is the key to a favorable outcome
Author Disclosure:
A. Vahabzadeh, None; M. A. Schleupner, None.