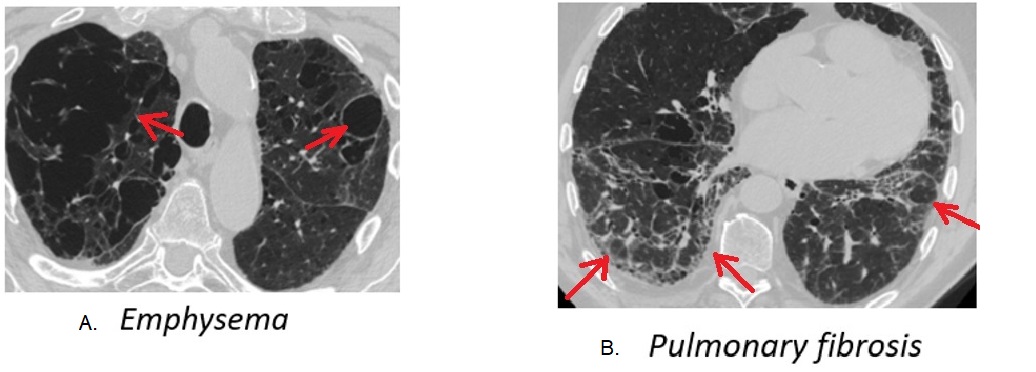
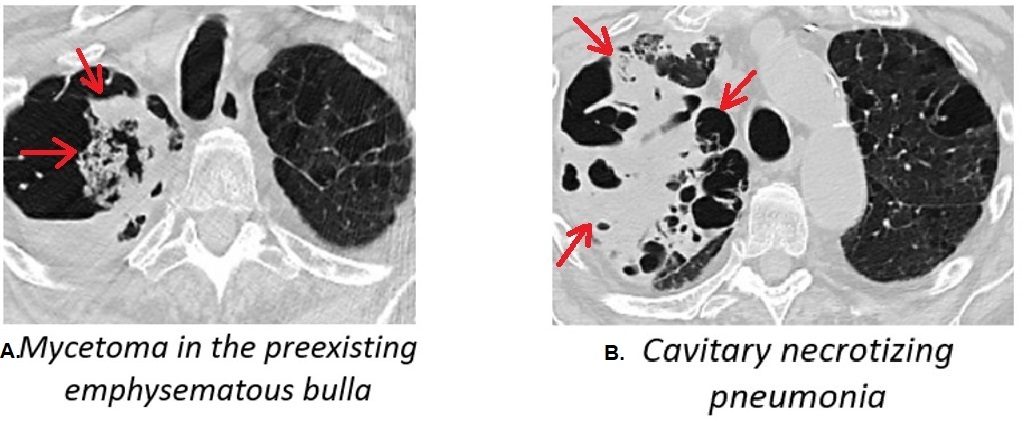
Case Presentation: An 87-year-old man presented to the emergency room for exertional dyspnea, productive cough, and generalized weakness progressive over the past month. Four weeks prior he was hospitalized for community-acquired pneumonia and received a 10-day course of a third-generation cephalosporin with minimal improvement. He continued to have a productive cough and exertional shortness of breath while in post-acute rehab. The patient had a background history of pulmonary fibrosis, bullous emphysema, and rheumatoid arthritis. He was taking prednisone 5 mg daily.On presentation, he was malnourished, tachypneic, and had a cough productive with copious amount of rusty sputum. Rales were heard in the middle and upper lobes of the right lung. Laboratory findings were remarkable for WBC of 22*10^9/L, and procalcitonin of 1.71 ng/L. The chest computer tomography demonstrated a large cavity in the right upper lobe with intraluminal ball-like opacity along the medial aspect. There was consolidation with thick wall cavitations seen in the right middle lobe. Bronchoalveolar lavage from the right upper bronchus sent for cultures grew colonies of Aspergillus niger. Serum galactomannan was 0.16 (cut off 0.5).The patient was initially treated with cefepime and vancomycin for hospital-acquired pneumonia, then metronidazole was added for possible ongoing aspiration. He was started on voriconazole on day 8 of admission when the positive fungal culture was received. The patient deteriorated during the hospital stay with progressive weight loss and fatigue. He opted for hospice and expired on day 13.
Discussion: Invasive pulmonary aspergillosis (IPA) has a high mortality rate and is one of the most common undiagnosed infections in intensive care unit patients. AIPA is routinely suspected in patients with prolonged neutropenia and stem cell transplant patients. SIPA however is rarely considered. More than that, SIPA comprises a diagnostical challenge due to an indolent clinical course, nonspecific imaging findings, and limited laboratory testing. Particularly bronchial cultures and PCR cannot differentiate between infection and colonization, galactomannan and beta-d-glucan have suboptimal sensitivity and specificity in immunocompetent patients, and tissue biopsies are often not obtained due to patients’ fragility. Clear-cut diagnostic criteria for SIPA do not exist. The high level of concern is crucial in patients with underlying structural lung disease and suspicious imaging findings, who do not respond to treatment with antibiotics in order to improve mortality.
Conclusions: It is important to increase clinicians’ awareness of SIPA in patients with underlying structural lung disease. Treatment with antifungal medications may improve clinical outcomes in particular clinical scenarios.