Background: Interprofessional education (IPE) has been shown to enhance knowledge, skills, and collaborative attitudes among healthcare providers, while also improving patient outcomes. While IPE is becoming more common in undergraduate medical education, many graduate medical education (GME) programs currently lack formal curricula. Those GME curricula that involve experiential learning have focused largely on the nursing role through shadowing experiences. However, medicine trainees work on large interprofessional clinical teams, which include nurses, physical and occupational therapists (PT & OT), respiratory therapists (RT), and speech and language pathologists (SLP), but many trainees lack knowledge of these other professions and effective understanding of interprofessional collaborative practice.
Purpose: In our large academic internal medicine (IM) program, we developed a novel IPE program to improve knowledge of 5 healthcare professions and thereby enhance interprofessional teamwork in the inpatient setting.
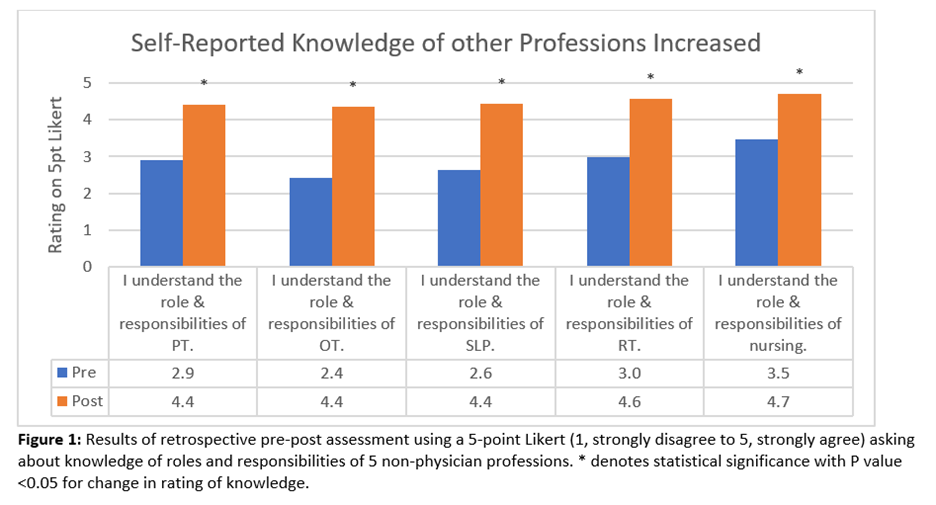
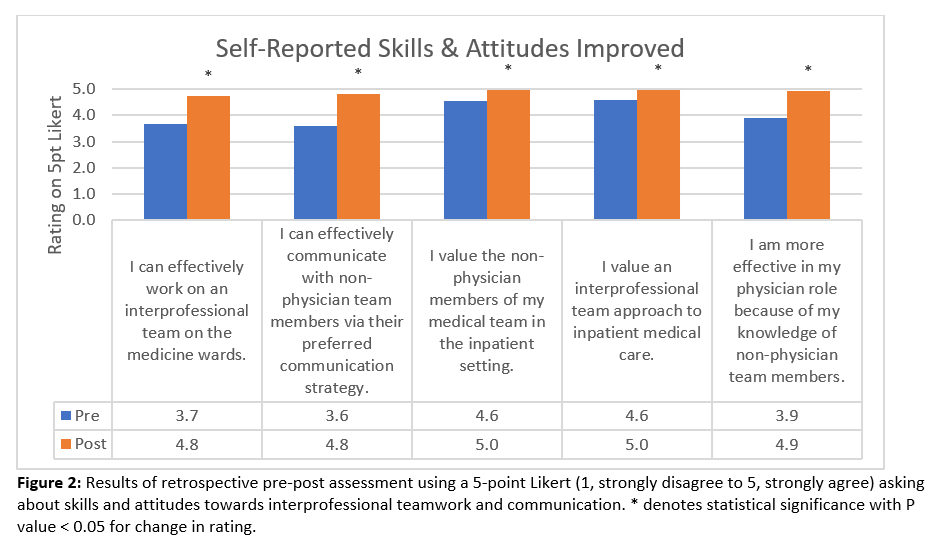
Description: The educational experience involved a 2-day curriculum for 49 PGY1 IM residents and included experiential learning and peer teaching during the ambulatory “Y week.” Each intern shadowed 1 of 5 healthcare professionals for 1.5-2.5 hours (Nursing, PT, OT, RT, and SLP) and was expected to complete a worksheet about the observed profession, which included education, workflow, responsibilities, and communication preferences. The following afternoon, the interns reported out on their shadowing experience and research, with a faculty facilitator guiding the discussion. Attendance was 98% at the shadowing experience and 100% at the report-out session. 100% of trainees completed the retrospective pre-post assessment instrument following the report-out session. Using a 5-point likert, trainees rated an increase in self-reported knowledge of the roles and responsibilities of each profession, with the lowest baseline knowledge and greatest increment in rating of self-reported knowledge for OT, followed by SLP (mean rating for PT 2.9 to 4.4, OT 2.4 to 4.4, SLP 2.6 to 4.4, RT 3 to 4.6, Nursing 3.5 to 4.7). Trainees also reported a high baseline rating of their value of non-physician team members on the inpatient medical team and value of an interprofessional team approach to inpatient medical care (mean rating 4.6 out of 5 for both). Trainees reported an increase in their self-reported ability to work on an interprofessional team (3.7 to 4.8), to effectively communicate with non-physician team members via a preferred communication strategy (3.6 to 4.8) and to be more effective in the physician role because of knowledge of non-physician team members (3.9 to 4.9).
Conclusions: This is a highly generalizable interprofessional education initiative, effectively built within the clinical learning environment and involving experiential learning and interactive flipped classroom peer teaching. Our novel IPE experience was built upon high baseline trainee reports of valuing interprofessional teamwork and valuing the non-physician members of the team. Our curriculum enhanced trainee-reported knowledge of the roles and responsibilities of other professionals on the clinical team and also enhanced trainees’ ability to work on the interprofessional team more effectively and to more effectively communicate with non-physician professionals on the team. This has the potential for sustained improvement in teamwork, communication, provider satisfaction, and patient outcomes.