Background: Many academic hospitalists begin their careers directly after residency and are expected to become teaching attendings without additional training or experience. Early attendings must quickly learn how to balance autonomy and supervision, advance patient care, and educate a wide spectrum of learners. Although tools such as faculty development workshops or peer observation programs are available to enhance teaching skills, their short durations and asynchronous formats may limit impact.
Purpose: To develop and launch a new coaching program for early-career inpatient teaching attendings focused on (1) developing skills in domains required of clinician-educators and 2) creating a more longitudinal experience grounded in practice-based learning.
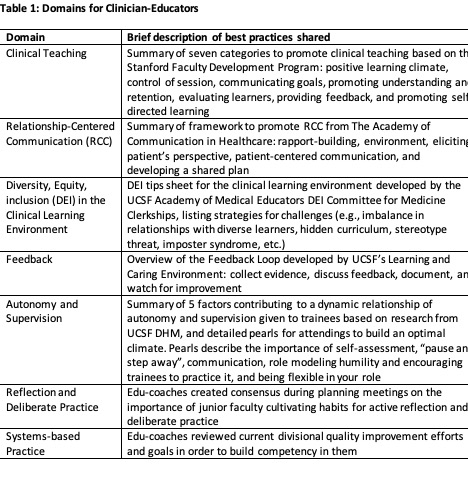
Description: This program was developed in a large (150+ faculty) division of hospital medicine based in an urban academic tertiary-care hospital. Hospitalists serve as teaching attendings for 8 resident-led teams comprised of interns and students for 9-10 days-long blocks. We first developed the structure and goals of this program, the “Master Educator Coaching Program” (MECP), by engaging with educational and administrative leaders in the division. We designated a director and identified 6 senior faculty with the highest divisional teaching evaluations. Over a 2-month design period, we obtained group consensus on 7 domains and best practices crucial to building mastery as an inpatient teaching attending (Table 1) and finalized a program structure.MECP was piloted during the July 2023 to June 2024 academic year. The inaugural class of junior attendings (“edu-coachees”) comprised 2 Internal Medicine chief residents and 3 hospital medicine fellows, all at the PGY4 or 5 level. Each edu-coachee was paired with a senior faculty coach (“edu-coach”). Clinical schedules were matched so that the pair co-attended during the edu-coachee’s first teaching block. Each pair met before their block to co-create shared goals and expectations.Co-attending practices largely involved the edu-coaches observing rounds most mornings, including the clinical care of patients, shadowing meetings with learners, and observing teaching. Each coaching pair then had a daily debrief to reflect, discuss progress, and provide feedback. Separately, the edu-coaches met regularly to share their experiences.Pairs were asked to complete surveys before and after the program to assess goals, challenges, confidence in domains, and impact. Division leadership continuously sought direct feedback, and survey results so far show the largest increases in edu-coachee confidence in: having an effective control of session, feedback to trainees, adjustment of autonomy and supervision, and advancing habits of reflection and deliberate practice (Table 2). Edu-coaches reflected on this experience with prominent themes including fresh perspectives on a new attending’s experience, expanding observation and feedback repertoire, personal behaviors aspiring to promote more trainee autonomy, and the unique and immense value of a longitudinal experience for a deeper coaching relationship.
Conclusions: We successfully launched an intensive co-attending coaching program that helped develop the confidence and reported skills of junior attendings in a relatively short period of time. Our coaching framework based on 7 domains allowed senior faculty to customize the structure to best meet each junior attending’s needs for effectual coaching.