Background: According to AHRQ, patient safety culture refers to the beliefs, values, and norms shared by health care practitioners and other staff throughout the organization that influence their actions and behaviors. Safety reporting (or incident reporting) is an important aspect of safety culture. Safety reporting of adverse events is a valuable epidemiological tool to measure the frequency of events and effectiveness of patient safety interventions. Despite assurances of anonymity and being non-discriminatory, reliable safety reporting has been hard to achieve, especially among clinicians. Safety reports captures contextual information about events that caused serious harm or occasionally ‘near misses’, which are rarely documented in medical records and yet occur more frequently than adverse events.
Purpose: To develop and foster a culture of safety within our group wherein safety reports are viewed as an opportunity to learn and improve ourselves.
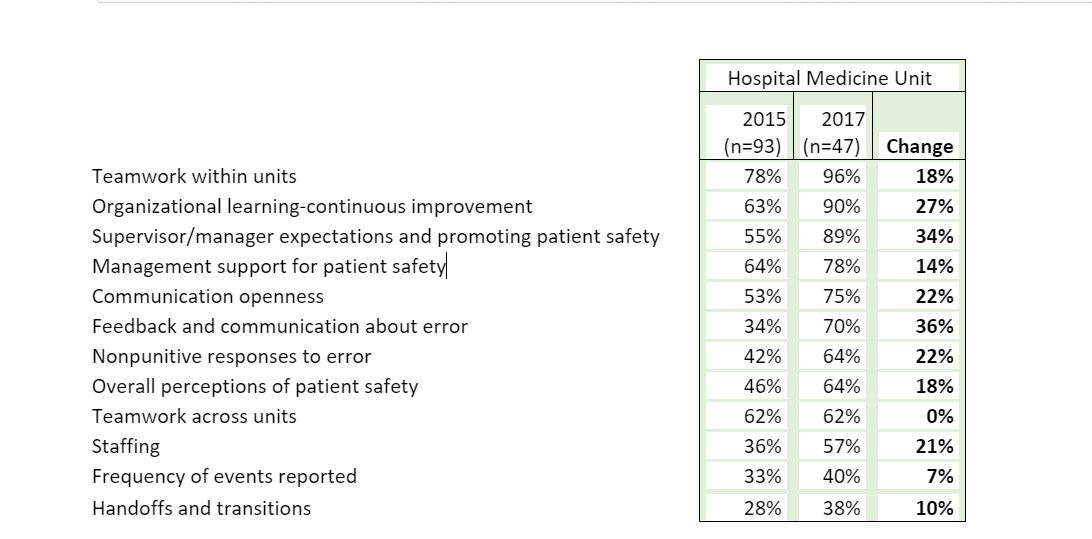
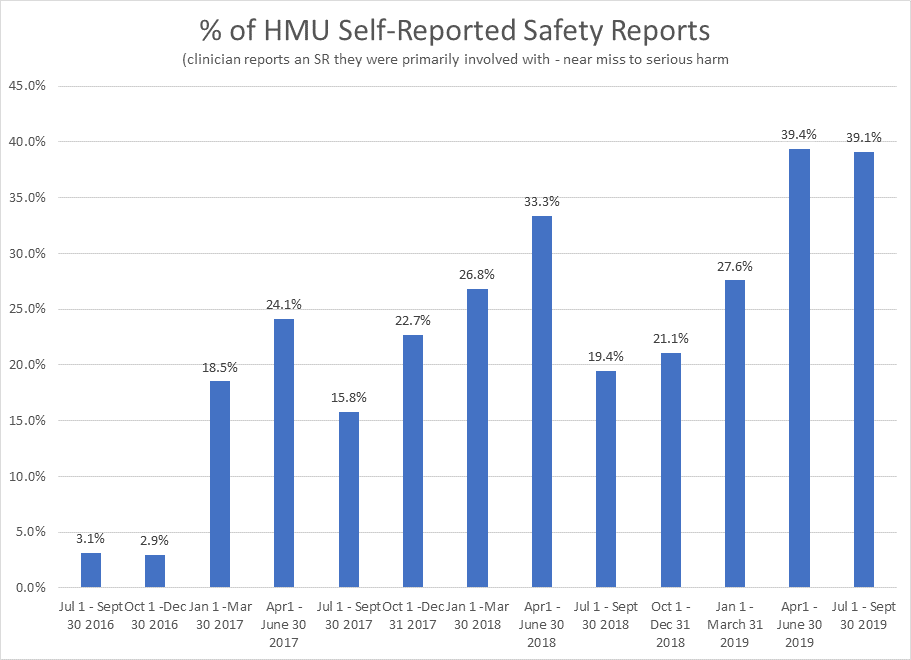
Description: Building a safety culture within an institution is challenging. It must be non-punitive, informative and maintain the commitment to confidentiality of the reporting clinician. We developed an initiative in 2016 to improve our safety culture through a series of interventions delivered via organized monthly meetings focusing on Just Culture. Interventions included: ensuring transparency of both the reporting and investigation process through multiple feedback mechanisms; emphasizing reports as learning opportunities; highlighting how reports translate into actionable change; and providing forums for staff to identify opportunities for improvement outside of incident reporting. The open meeting setting nurtured an environment where incident reports became an educational tool free of punitive stigma. Safety culture is objectively measured by the SOPS survey designed by AHRQ, which at our institution is conducted every 2 years. It consists of 48 questions which are divided into 12 domains. Since implementation in 2016, we have improvement in 71% of questions in the SOPS survey with an average absolute improvement of 25% per question and 19% per domain from 2015 to 2017. The Department of Medicine and overall Hospital improved 6% and 3% on average for each of the 12 domains over the same time period. During this improvement and between SOPS surveys, we created and tracked a novel metric of safety culture, the % of safety reports that were self-reported (i.e., a clinician ordered the wrong medication and submitted an incident report, rather than someone else submitting an incident report). We observed a substantial improvement in the rate of self-reported incident reports without any change in the overall amount of incident reports attributable to our Unit. The baseline rate of clinician self-reported safety reports was approximately 3.0% in the first two quarters after starting our intervention, and steadily increased to approximately 40% as per the last measure in September 2019. The increase in this metric in early 2017 coincided with the improvements noted in the SOPS survey from the same time period.
Conclusions: Organized meetings to discuss safety reports as a comprehensive strategic initiative favorably transforms the patient safety culture of the clinicians in our Hospital Medicine Unit. Patient safety culture can be monitored in near-real time via a novel metric that correlates with AHRQ SOPS survey results.