Background: Sepsis is a common and life-threatening complication of infection that disproportionately affects patients with chronic comorbidities. Timely fluid resuscitation is a key initial management strategy for reducing sepsis mortality; however, patients with serious comorbidities are often excluded from clinical trials. The Surviving Sepsis guidelines suggest that patients meeting severe sepsis criteria should be administered fluids starting at least 30cc/kg in initial management; however, data is lacking for patients with congestive heart failure (CHF) where the complication of pulmonary edema is a common concern. We sought to determine the practice patterns of volume of fluid administered among septic patients with and without CHF and to identify the association between initial volume of fluid administered and clinical outcomes.
Methods: We performed a retrospective cohort study at an academic medical center extracting data from the Electronic Health Record (EHR) all adult patients presenting to a single academic emergency department (ED) between June 2012 to December 2018 who met validated Sepsis-III EHR criteria and had an initial lactate of at least 2 mmol/L. Patients with CHF were identified using ICD-10 codes. The medication administration record was used to calculate fluids administered in the first 24 hours following ED presentation. Multivariable regression, adjusted for demographics, comorbidities, triage vitals, total SOFA score, and initial lactate and lab values, was used to estimate associations with in-hospital mortality and mechanical ventilation per additional liter of total volume in the first 24 hours separately in patients with and without CHF.
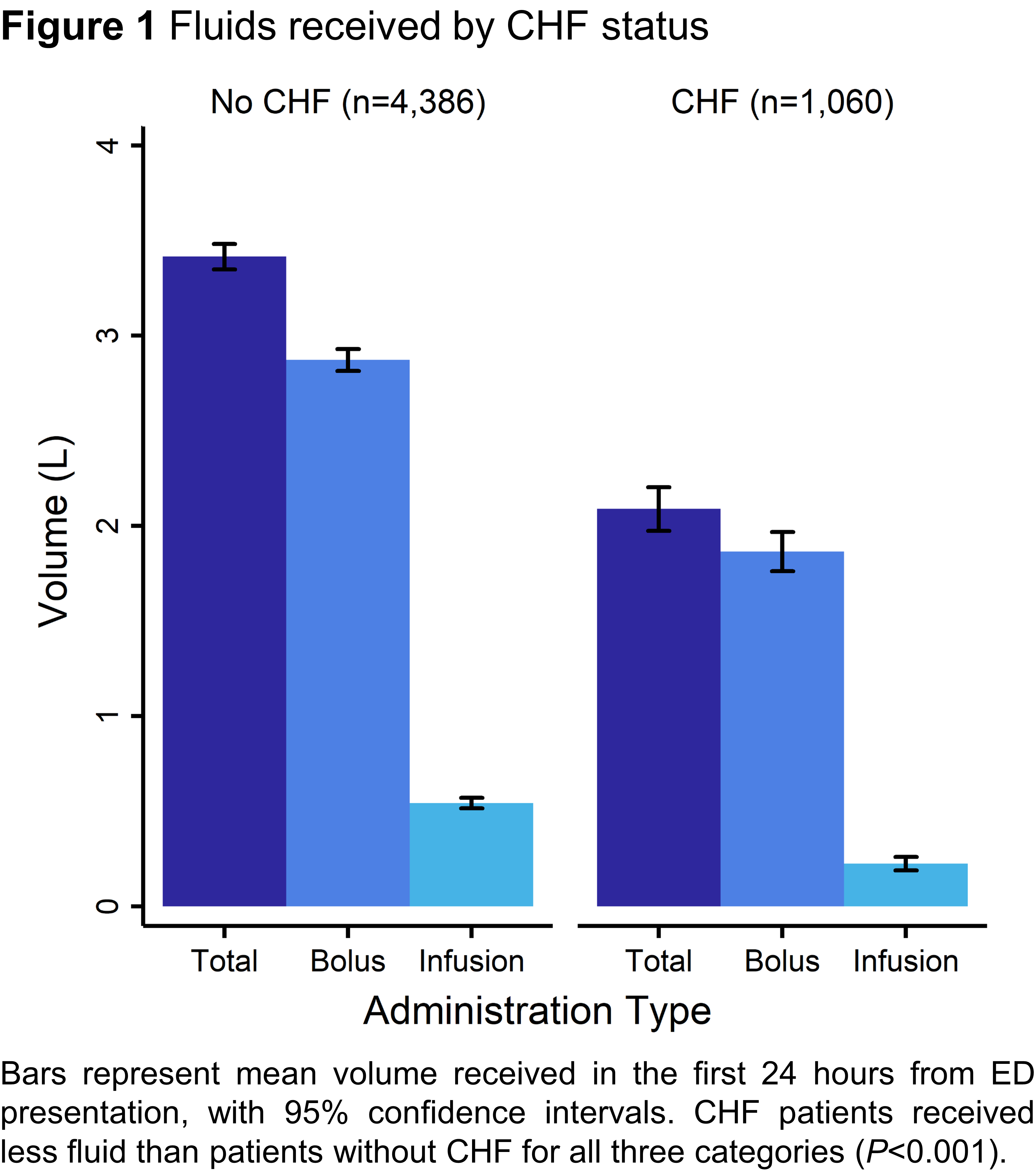
Results: Patients with CHF (n=1,060, 19.5%) received less fluid overall (CHF mean 2.1 ± 1.9L vs. no CHF 3.4 ± 2.2L, P<0.001) compared to those without CHF (n=4,386) in the first 24 hours (Figure). In multivariable regression models, every additional 1L fluids in the first 24 hours was associated with decreased likelihood of death in patients without CHF (OR=0.86, 95% CI 0.81–0.90, P<0.001) but there was no association in those with CHF (OR=0.94 95% CI 0.85–1.03, P=0.18). In a similar model, there was no significant association with need for mechanical ventilation among patients with CHF (OR=1.02 95% CI 0.89–1.18, P=0.77) or without (OR=1.03 95% CI 0.98–1.08, P=0.29).
Conclusions: In this observational study, we found that clinicians are administering lower fluid volumes to patients with history of CHF. While increased fluid administration in sepsis is associated with decreased mortality in patients without CHF, this was not observed in the CHF patients. There was no association with need for mechanical ventilation in either group. These findings suggest that while CHF patients may not benefit from guideline-appropriate levels of fluid resuscitation, the harms of increased mechanical ventilation were also not observed. More investigation is needed to determine the optimal fluid resuscitation strategy in patients with CHF.