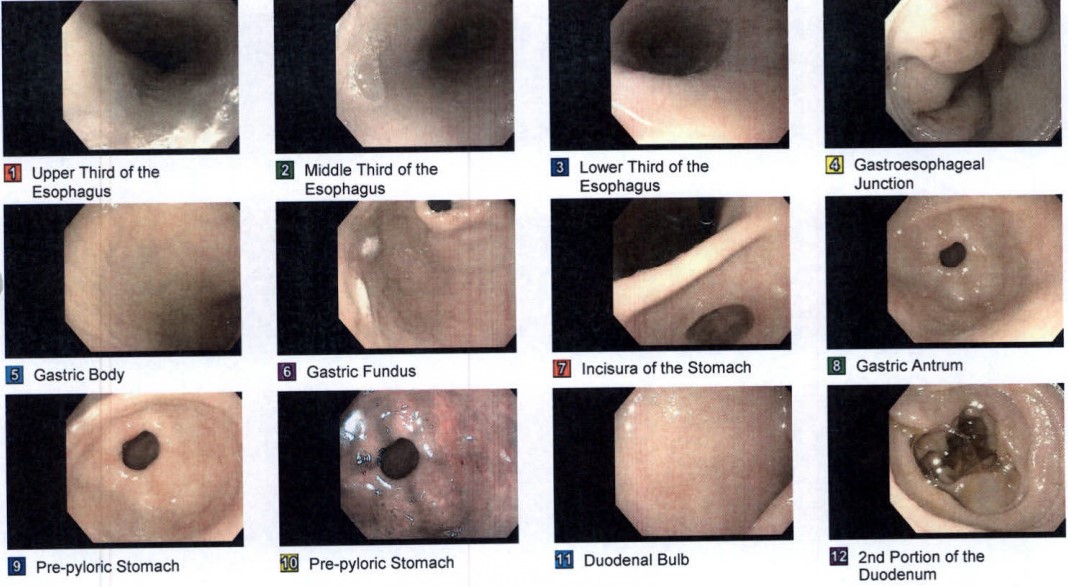
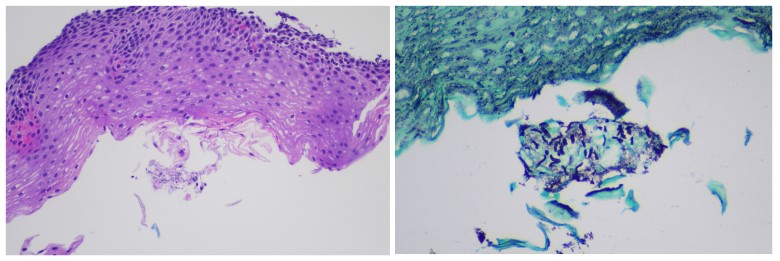
Case Presentation: A 58 year-old female with a history of pre-DM, HTN, cholelithiasis s/p cholecystectomy, and GERD presented to the clinic with a chief complaint of odynophagia. Symptoms began 3-4 days prior and were located primarily in the lower chest. The pain started abruptly with no precipitating factor and, while not worsening, was not improving. The pain was described as a 6/10 ache that’s episodic and, primarily associated with solid food intake. The episodes of pain lasted for a few minutes after eating and were accompanied by a sensation that the food was ‘stuck’. She denied fever, chills, nausea/vomiting, bad breath, foul taste in mouth, voice hoarseness, cough, and weight changes. She denies ever smoking. She had a recent endoscopy within the last year for persistent GERD with biopsy results consistent with reflux esophagitis. She has not used a PPI for the last year but was taking famotidine daily. Age-appropriate cancer screens were up to date (colonoscopy, mammogram, cervical), and she denied any personal or family history of cancer, or recent corticosteroid use. She has not been sexually active in 10 years and had a previous HIV screen that was negative. Vital signs were unremarkable and the physical exam, including oral, was unrevealing except for mild epigastric tenderness on deep palpation.She was initially prescribed a proton pump inhibitor (PPI) given unclear etiology of acute odynophagia with close follow up within a few weeks to assess her response. She was instructed to follow up with her Gastroenterologist or call the clinic to schedule an earlier appointment if symptoms persist or worsen. The odynophagia did not resolve and the patient ultimately followed up with her Gastroenterologist. An endoscopy was performed which revealed LA Grade A esophagitis at the gastroesophageal junction as well as patchy mild gastropathy in the gastric antrum but no clear etiology (Figure 1). Biopsy revealed lymphocytic inflammation and pseudo hyphal forms compatible with Candida esophagitis (Figure 2). Repeat CBC and HIV tests were unremarkable. She was started on 14 days of fluconazole with resolution of symptoms.
Discussion: Candida esophagitis is the most prevalent form of infectious esophagitis and accounts for roughly 88% of infectious esophagitis. Patients may be asymptomatic or may have dysphagia, odynophagia, and retrosternal pain. Candida esophagitis tends to be associated in patients who are immunocompromised. In immunocompetent patients, studies have shown the use of PPIs and H2 antagonists to be associated with Candida esophagitis. Guidelines recommend systemic antifungal therapy for the treatment of Candida esophagitis.
Conclusions: Candida esophagitis is traditionally associated with an immunocompromised state and is a common differential in the evaluation of odynophagia in an immunocompromised patient. Here, we present a rare case of an immunocompetent patient with recent use of H2 antagonist who presented with acute odynophagia and was found to have candida esophagitis on endoscopy. She was successfully treated with systemic antifungal therapy. In nonimmunocompromised patients, Candida esophagitis should be considered as a possible differential for the patient who presents with acute odynophagia particularly if they are on acid suppressing therapies.