Background: Hospitalists commonly discuss advance care planning (ACP), which supports patients in understanding and expressing their values for medical care during serious illness. The coronavirus disease of 2019 (COVID-19) pandemic has increased the urgency of these conversations, especially for patients with older age, comorbidities, or an otherwise high risk for complications such as ICU admission, mechanical ventilation, or death. Unfortunately, the COVID-19 pandemic has posed challenges to having ACP discussions, such as reduced in-person visits and hospital visitor restrictions. Little is known about patterns of ACP discussions during the COVID-19 pandemic. In this study, we sought to describe the frequency, quality, and predictors of ACP documentation among patients hospitalized early in the COVID-19 pandemic.
Methods: This retrospective observational study included all adults tested for COVID-19 and admitted to a large academic medical center between March 1-31, 2020. During this time, COVID-19 testing was performed based upon clinical suspicion for infection. As part of a health system-wide initiative preceding the pandemic, providers were instructed to document ACP conversations within an ACP navigator, an easily accessible area of the electronic medical record that centralizes ACP documentation, code status, and advance directives. In this study, ACP documentation was defined as documentation within the navigator. Data were abstracted by structured chart review and reconciled by two independent physician reviewers. Differences in sociodemographic factors, clinical characteristics, and ACP documentation were analyzed using unpaired t tests for continuous variables and Fisher’s exact tests for categorical variables. Multivariate logistic regression was used to identify factors associated with ACP documentation.
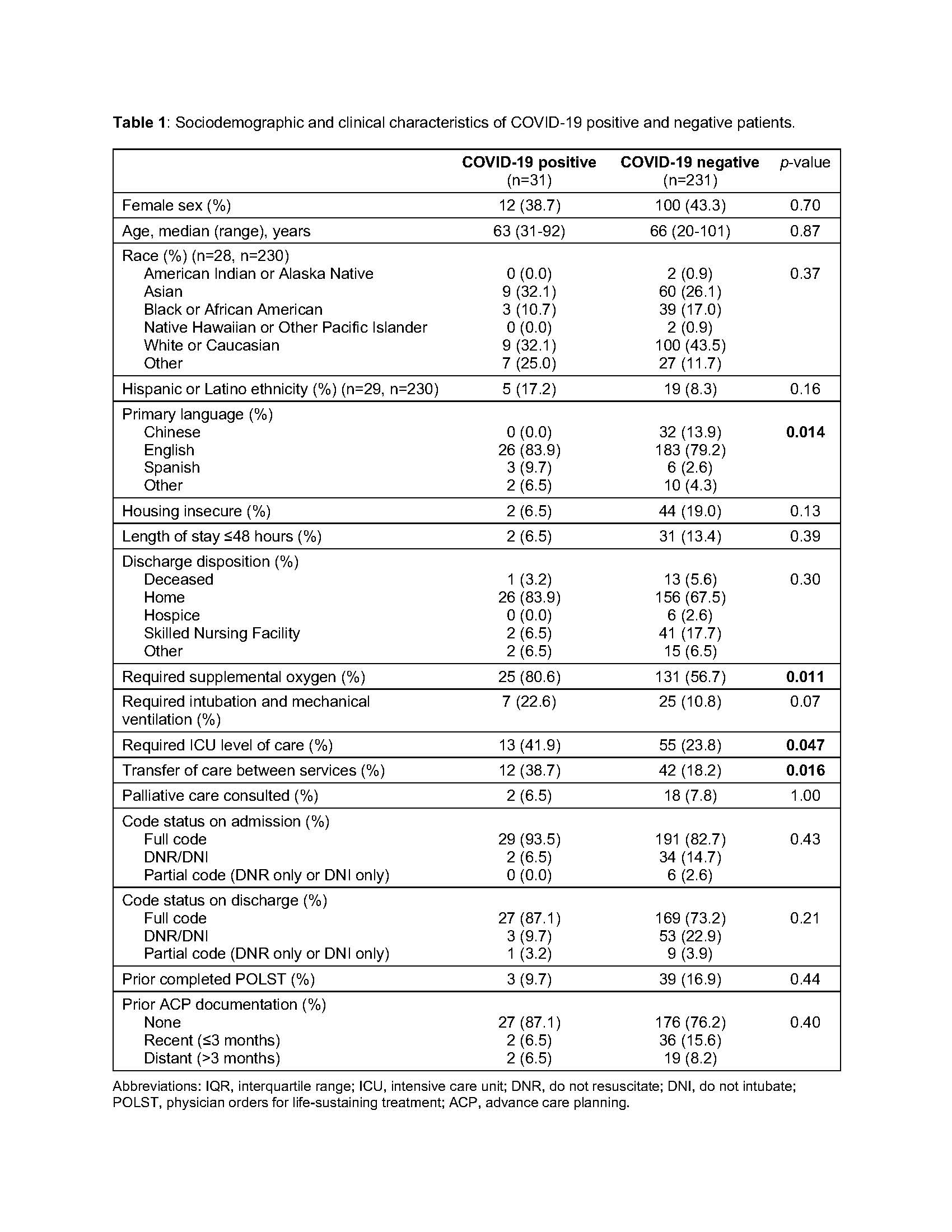
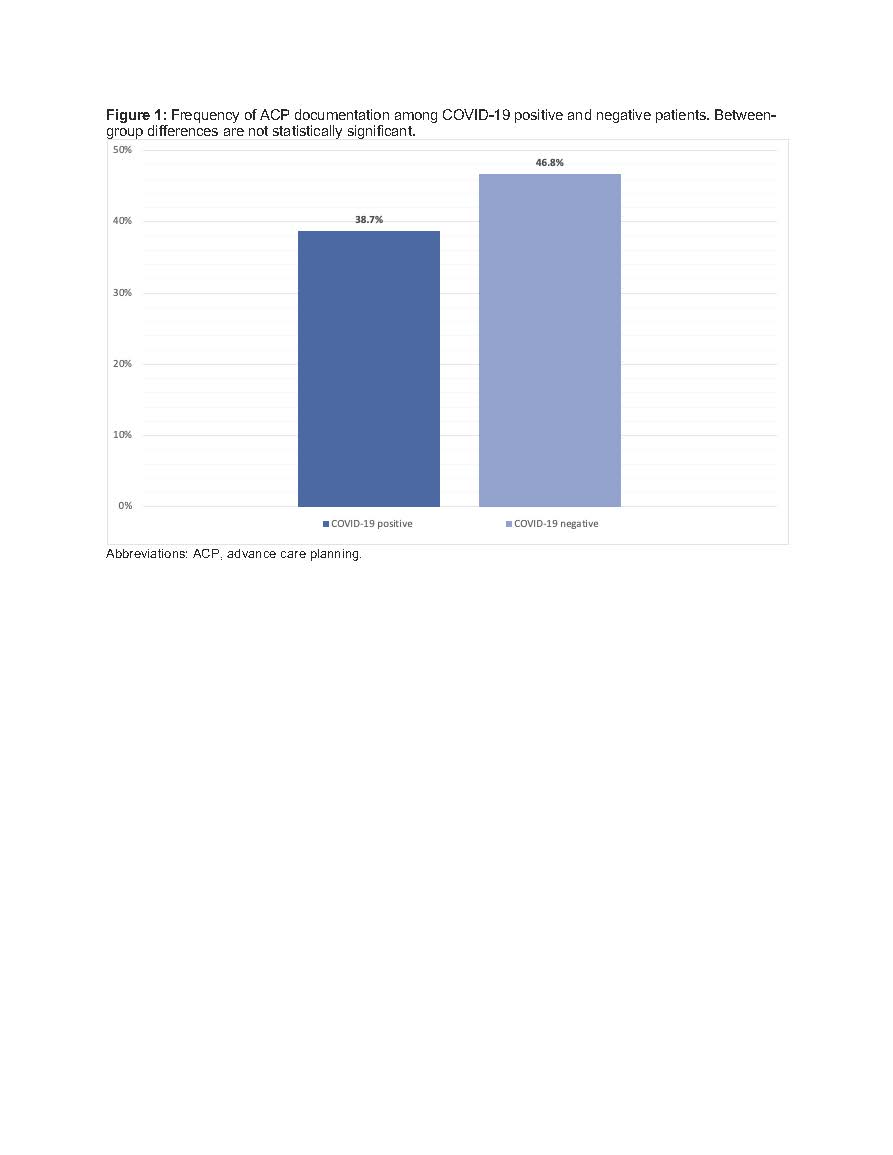
Results: Of 262 patients tested for COVID-19, 31 (11.8%) tested positive (COVID-positive). Sociodemographic and clinical characteristics are shown in Table 1. COVID-positive patients were more likely to require supplemental oxygen and ICU care. Overall, 12 (38.7%) patients with COVID-19 had ACP documented prior to discharge or death, compared to 108 (46.8%) patients without COVID-19 (Figure 1, p = 0.45). Comparing ACP documentation among COVID-positive and COVID-negative patients, there were no significant differences in documentation of code status (100% vs 94.4%), surrogate decision-maker (58.3% vs 66.7%), prognosis (8.3% vs 29.6%), or other treatment wishes (41.7% vs 62.0%). Among all patients, palliative care consultation (OR: 6.93, p=0.004), non-full code status on admission (OR: 5.79, p<0.001), length of stay over 48 hours (OR: 5.25, p=0.002), housing security (OR: 2.28, p=0.043), and older age (OR: 1.03 for each year increase, p=0.002) were associated with ACP documentation.
Conclusions: Hospitalized patients with and without COVID-19 had similar rates of ACP documentation, with fewer than half of patients having ACP discussions documented. Most ACP notes identified code status or surrogate decision-maker, but few addressed prognosis. Factors associated with ACP documentation included palliative care consultation and non-full code status on admission. These findings reinforce the urgency of ACP conversations for COVID-positive patients and a potential role for palliative care consultation. While hospitalists should always aim to provide goal-concordant care for their patients, these needs are magnified by the ongoing COVID-19 pandemic.