Case Presentation: A 57 year old man with a history of heart failure with preserved ejection fraction (HFpEF), chronic kidney disease (CKD) and hypertension presented with two weeks of exertional dyspnea and lower extremity edema, followed by 4-days of progressive tongue swelling. One-month prior, he was initiated on an ACE inhibitor (ACEi) and experienced tongue swelling 2 weeks later. He received a course of steroids at that time with resolution of his symptoms. Physical exam revealed normal vital signs, macroglossia with mild glottic edema and pitting edema of both lower extremities. He was diagnosed with recurrent ACEi associated angioedema. The ACEi was discontinued; Anti-histamines and steroids were implemented and provided marked symptomatic relief. A transthoracic echocardiogram performed to evaluate his hypervolemia revealed an abnormal myocardial texture, new systolic dysfunction and a restrictive cardiomyopathy, concerning for Amyloidosis.
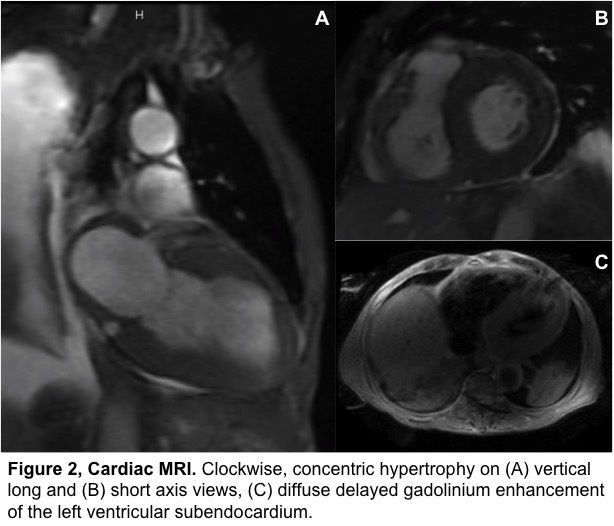
Labs demonstrated nephrotic range proteinuria, elevated IgG-lambda monoclonal proteins and elevated lambda free light chains. Abdominal fat pad biopsy results were inconclusive and PETCT did not find any osseous lesions. The patient soon developed cardiogenic shock due to multiple conduction abnormalities. Attempts at bone marrow and endomyocardial biopsy were abandoned given his tenuous hemodynamic status. A cardiac MRI was consistent with amyloidosis. Unfortunately, our patient’s advanced cardiac involvement precluded initiation of any targeted therapy other than doxycycline.
Discussion: Light chain amyloidosis (AL) is a plasma cell dyscrasia characterized by the overproduction, misfolding and extracellular deposition of immunoglobulin light chain. Here we present a case of AL amyloidosis presenting with recurrent macroglossia misdiagnosed as angioedema. ACEi use, unclear chronicity of HFpEF and CKD confounded the diagnosis. Multi-organ involvement is common, however advanced cardiac disease precludes the use of many effective therapies. Hence, early recognition by hospitalists and initiation of targeted therapy is imperative, as any delay may prove dire.
Despite the advances in AL amyloidosis treatment, 1-year mortality remains high in large part due to under recognition of the disease leading to delays in diagnosis. Early cardiac manifestations are often subtle with nonspecific ECG findings such as low voltages and poor R wave progression. Early restrictive cardiomyopathy can also be mistaken for diastolic dysfunction on echocardiography. Stem cell transplantation (SCT) and induction chemotherapy have been well studied to improve survival in AL Amyloidosis. However, advanced heart failure is a relative contraindication to SCT and certain chemotherapies due to increased mortality.
Conclusions: This case illustrates the importance of considering AL amyloidosis in patients with presumed HFpEF, especially in light of nephrotic syndrome in the absence of diabetes. Hospitalists should keep amyloidosis on their differential diagnosis in similar patients. This case underscores the subtle presentation and difficult diagnosis of AL amyloidosis, its aggressive nature and the consequences of delayed recognition.
.jpg)