Case Presentation: A 78-year-old African-American male with a history of paroxysmal atrial fibrillation, syncope, hypertension, and heart failure with reduced ejection fraction (HFrEF 30-40%) presented to the emergency department with increased exercise intolerance and shortness of breath. In addition, he reported progressive leg swelling and episodic chest pressure. Vitals were within normal limits (BP 106/71, RR 14, HR 70; T 98F) Physical exam was significant for a non-obese male with +1 JVD, + 1 bilateral lower extremity edema, and inspiratory crackles.
Labs were significant for a troponin (0.27) and BNP (389) that were higher than his baseline (0.14 and 300). Furthermore, persistently elevated troponin (mean 0.145) was noted for approximately 10 years, 5 years before his HF diagnosis. All other labs including kidney and liver function, hematology, and urine drug screen were normal. Chest X-ray revealed no acute cardiopulmonary abnormalities. EKG showed normal sinus rhythm with low voltage but no signs of ischemia. The patient was admitted for management of non-ST elevation myocardial infarction.
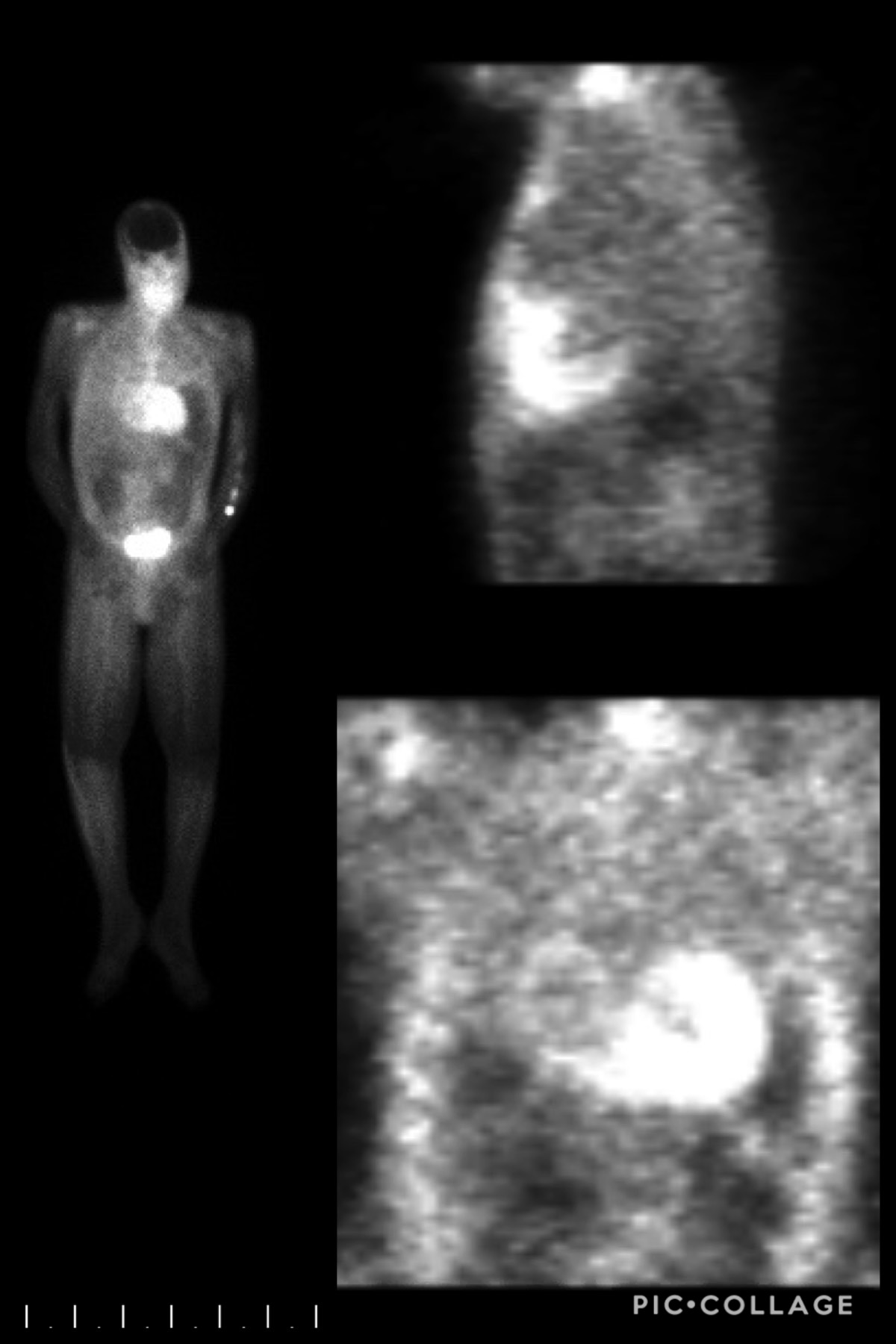
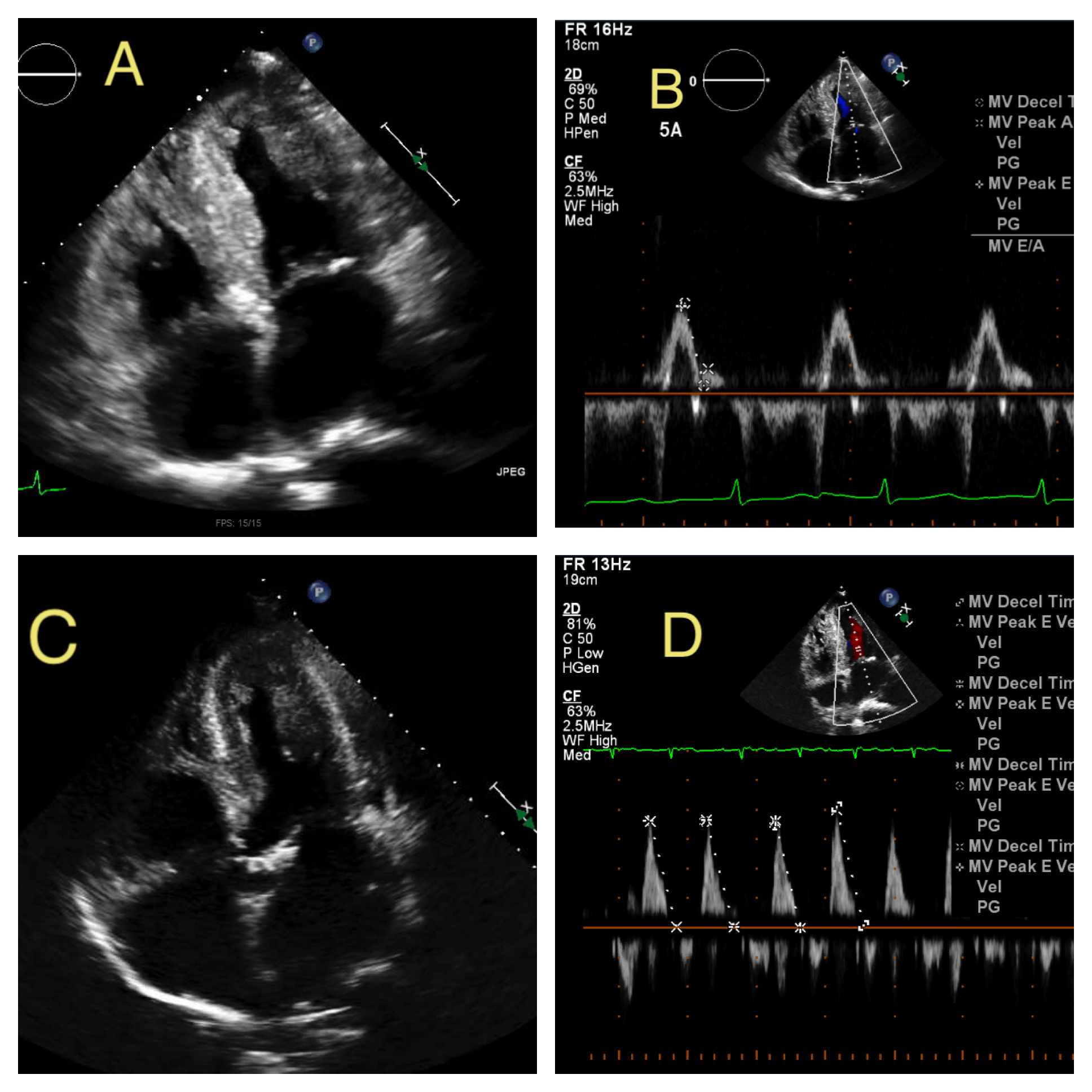
Transthoracic echocardiography (ECHO) was obtained which revealed a progressive decline in left ventricular ejection fraction (LVEF) to 25-35% along with worsening diastolic dysfunction with E/A 3.5 and medial E/E’ 24 despite patient’s adherence to medical management. ECHO at HF diagnosis (3-years prior) showed LVEF 50-55% and mild diastolic dysfunction E/A 0.78. Repeat ECHO 1.5 years prior revealed a decline in LVEF to 30-40%. Cardiac MRI was performed to rule out apical ventricular thrombi and showed diffuse late gadolinium enhancement concerning for amyloidosis. Follow up nuclear bone imaging revealed increased cardiac uptake greater than bone, suggestive of grade III cardiac amyloidosis. Fat pad biopsy and mass spectrometry confirmed tissue transthyretin amyloidosis. The patient was managed conservatively with diuretics and discharged with appropriate follow ups in place. His home lisinopril and metoprolol were discontinued due to concerns that they may worsen amyloidosis symptoms.
Discussion: Persistently elevated cardiac biomarkers may be of prognostic value in patients who do not respond to normal HF therapies and have rapid disease progression. Studies have shown that these markers may also be of diagnostic significance and help to differentiate cardiac amyloidosis from other causes of heart failure. In addition, this case illustrates the fact that more frequent ECHOs may be necessary to monitor disease progression in this patient population.
Conclusions: Troponinemia might play a role in the early diagnosis of Cardiac amyloidosis, however this needs to be further investigated.