Background: Facing challenges of capacity strain, many hospitals have implemented programs to prioritize discharges in the morning as a strategy to improve patient throughput, decrease emergency room boarding, and improve patient satisfaction/experience. (1) However, evaluations of these practices have had mixed results. (2) Like many other complex health interventions, priority discharge interventions may fail to improve downstream outcomes when deployed in real-life clinical settings; a priori, they must involve proactive planning and engagement of all members of the patient care team. Conceptualizing Discharge By Noon (DBN) programs as a complex health intervention (CHI) is an important first step to understand the mechanisms by which these programs do or do not succeed. In this study, we accomplish foundational work relevant to DBN programs by using a CHI framework to define the core functions (the intervention’s effectiveness-driving features) from its forms (the strategies used to deliver the core functions).
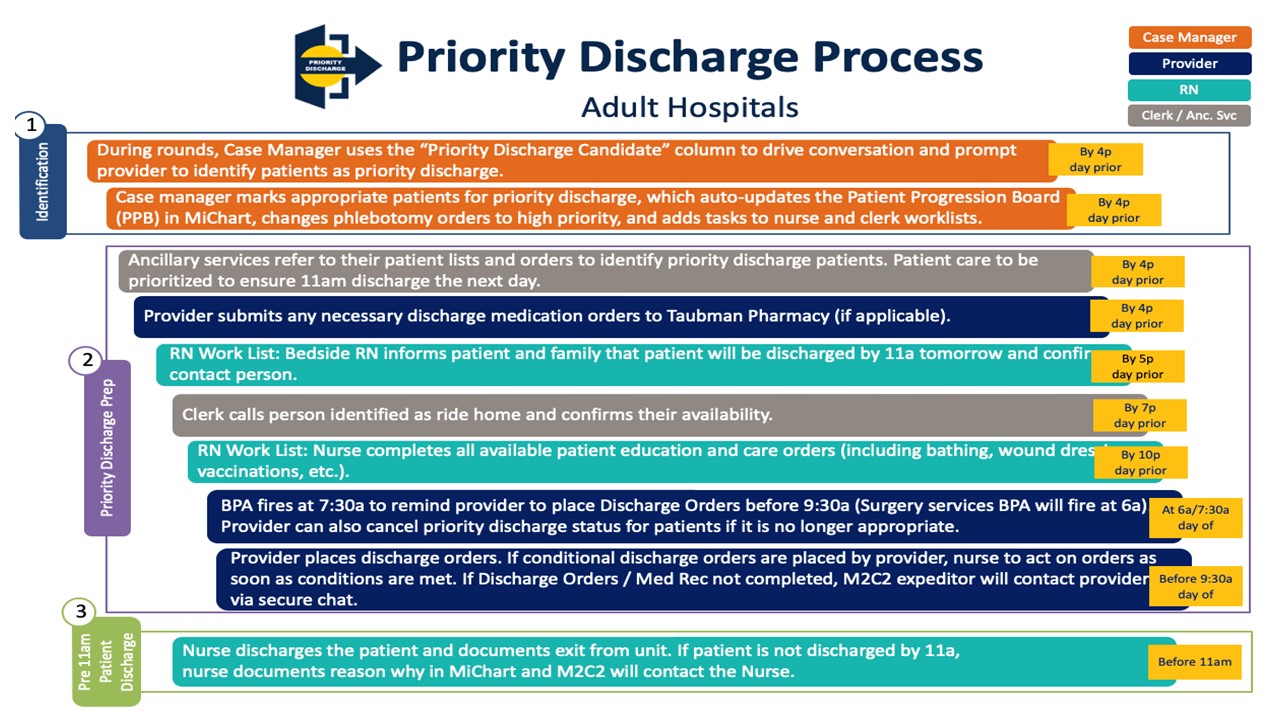
Methods: We used validated methods to identify core functions of a mature DBN program at an academic medical center. We first reviewed existing materials used in the development and implementation of the DBN program at the University of Michigan’s flagship academic hospital (1100 beds) and at the affiliated off-site hospital medicine inpatient unit at Trinity Health Ann Arbor (26 beds), to create a document describing DBN forms. We then surveyed multidisciplinary stakeholders involved in the development and/or implementation of DBN with the objective of distilling DBN forms into core functions. Interviews assessed 1) the system/patient need motivating the intervention, 2) the purpose and role of each aspect of the intervention, 3) the aspects of the intervention that were perceived to be essential to its success, and 4) methods and conditions necessary to implement the intervention. Two authors pilot coded the first three surveys inductively, and then a third member reviewed. The codes were discussed and finalized. The remainder of the surveys were coded to create a DBN Function and Form matrix. Additionally, each step in the priority discharge process (including day before and day of responsibilities, by stakeholder role) was disseminated at or prior to survey completion. (Figure 1)
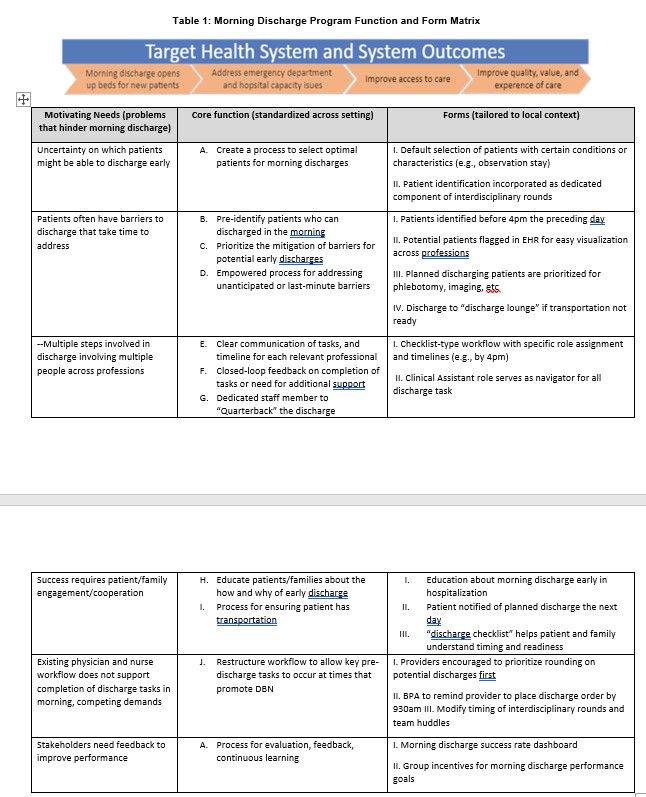
Results: Twenty-two of 23 (96%) stakeholders responded to the survey. Table 1 shows the DBN function and form matrix which includes: (a) problems that the care model seeks to address, (b) standardized core functions, and (c) customized forms. We included representative examples of forms to illustrate this area of the matrix for each core function. We identified 11 core functions addressing 6 motivating needs.
Conclusions: Our DBN Functions and Forms matrix supports an explicit theory-based depiction of how the intervention achieves its effects. It enables assessment of DBN programs’ fidelity (i.e., having all functions). Finally, it can be used for dissemination and scale-up for DBN programs by clearly distinguishing forms (which can be adapted to local context) from functions (which must be preserved across context).