Background: Increasing numbers of young adults are hospitalized in nonpsychiatric facilities for acute mental health crisis, such as suicide ideation (SI) or attempt (SA). We sought to evaluate differences in care quality and outcomes when these patients are admitted to the medical units of adult versus pediatric hospitals.
Methods: We retrospectively collected demographic and clinical data on patients aged 18-25 years old who were admitted to either the 550-bed adult (AH) or 348-bed pediatric hospital (PH) of a tertiary-care academic health system from 9/2017-6/2023 for SI, SA, or self-inflicted harm. We excluded patients directly admitted to the psychiatric unit and subsequent readmissions during the study period. Clinical data collected included admission for SA, Charlson comorbidity index score, time spent in ICU, ED and hospital length of stay (LOS), and use of psychiatry or psychology consultation. Primary outcomes included discharge to psychiatric hospital, post-discharge emergency department (ED) visit, and hospital readmission. Associations between the type of hospital (AH vs PH) and primary outcomes were evaluated via univariate analysis.
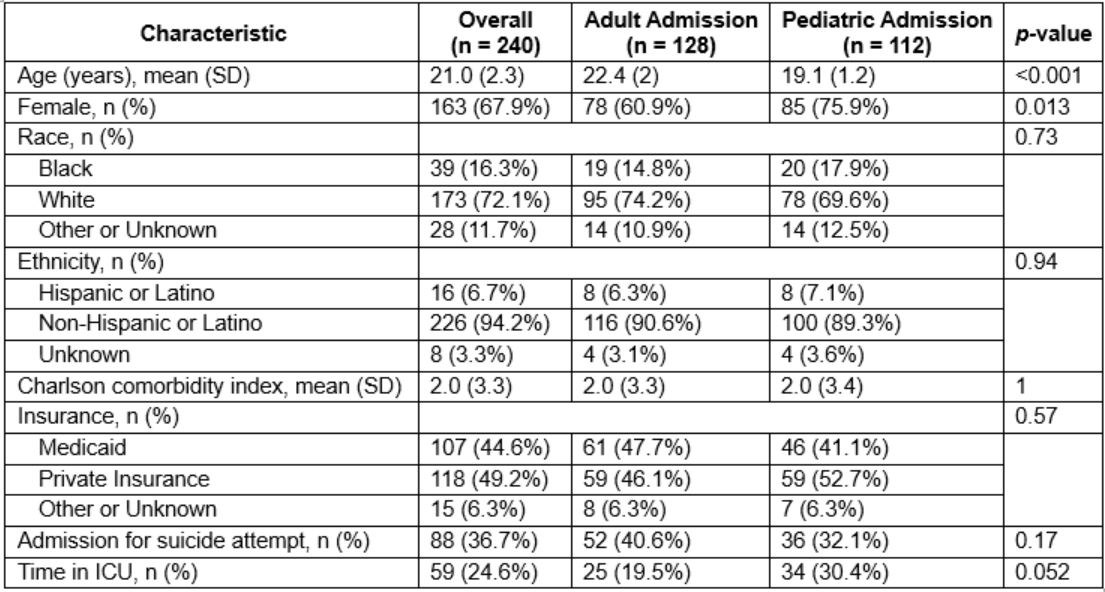
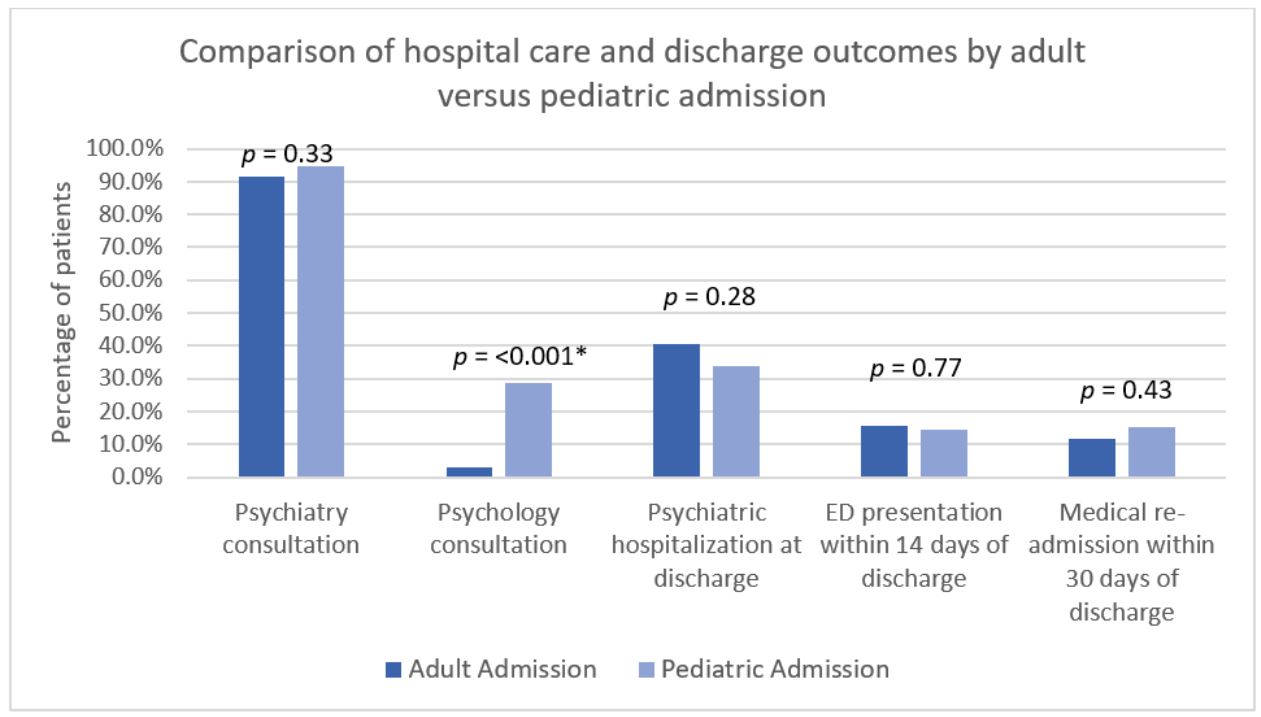
Results: Of 240 patients included, 128 (53%) were admitted to AH and 112 (47%) to PH. Overall, SA was the reason for admission in 88 (36.7%) encounters, which accounts for 40.6% of those in AH and 32.1% in PH (p =0.17). Compared to those admitted to PH, patients admitted to AH were older (22.4 vs 19.1 years old, p< 0.0001) and less likely to be female (60.9% vs 75.9%, p = 0.013) with similar comorbidity score (Table 1). While patients in AH had longer average ED LOS prior to admission (18.9 vs 9.6 hours, p = 0.005) there was no difference in average hospital LOS (198 vs 184.7 hours, p = 0.69). Nearly all patients had psychiatry consultation (92.9%), with similar rates in both AH and PH (91.4% vs 94.6%, respectively, p=0.33), but patients in PH had higher rates of psychology consultation (28.6% vs 3.1%, p < 0.0001). There was no difference in rates of discharge to psychiatric hospital, post-discharge ED visit, or hospital readmission (Figure 1).
Conclusions: In this single system study, young adults hospitalized for SI or SA received similar care and had similar outcomes regardless of admission to an adult or a pediatric hospital. Further work is needed to determine if observed differences in ED LOS and psychology consultation are generalizable and to assess how these differences affect hospital throughput and long term outcomes.