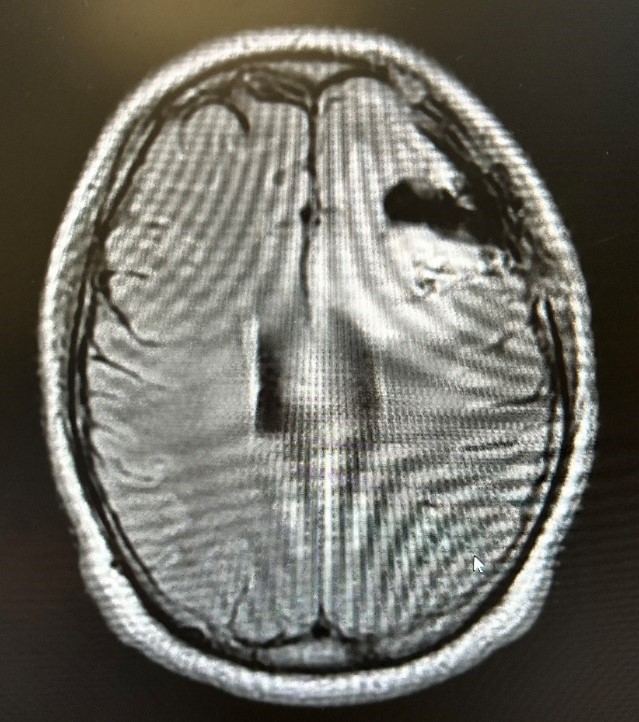
Case Presentation: This report presents a rare case of cefepime-induced neutropenic fever in a 25-year-old male with a history of frontal lobe arteriovenous malformation (AVM), status post surgical resection, and meningitis. The patient had no prior hematologic abnormalities. His previous admission was for new-onset seizures and severe headaches lasting 3 months. CT imaging revealed a left frontal lobe AVM, which was resected via craniotomy. Post-operatively, he developed leukocytosis (32,000) with associated fever. A repeat head CT showed an enlarging subgaleal fluid collection, and a lumbar puncture (LP) revealed >2000 WBCs (83% neutrophils), hypoglycorrhachia, and a gram stain showing PMNs, suspicious for meningitis. The patient underwent a second surgery for wound cultures, washout, and bone flap removal. Wound cultures grew Klebsiella, which was sensitive to cefepime. He was discharged with a plan for 6 weeks of outpatient cefepime therapy (2g q8hrs).During this admission, the patient presented with chills and a high-grade fever on day 3 of cefepime therapy, additionally was hypotensive and tachycardic which responded with fluid bolus. Laboratory tests revealed neutropenia with an absolute neutrophil count (ANC) of 350 cells/mm³, significantly lower than baseline. Infectious Disease and Neurosurgery teams were consulted for further infectious work up. After an active discussion, cefepime was replaced with meropenem. By day two of admission, the patient’s symptoms began improving. Neurosurgery removed staples from his scalp and confirmed the MRI findings were consistent with post-surgical changes. A repeat LP showed improved results compared to the prior admission, ruling out infection. The patient was stable for discharge on outpatient ertapenem 1g.
Discussion: This case highlights the potential for hematologic side effects in patients on prolonged cefepime therapy. Cefepime, a fourth-generation cephalosporin, is widely used for serious infections but can rarely cause neutropenia and subsequent neutropenic fever. The incidence of neutropenia with beta-lactam antibiotics is approximately 10% within the first two weeks of use. Neutropenic fever specifically due to cefepime is rare, with an estimated incidence of about 1%. The exact mechanism remains unclear but is believed to involve an idiosyncratic immune-mediated response that suppresses bone marrow production of neutrophils.
Conclusions: While cefepime is generally well-tolerated, it can, in rare cases, cause neutropenic fever. Clinicians should be vigilant for unexplained neutropenia with fever during cefepime therapy. In such cases, discontinuation of the drug and initiation of supportive care is essential to prevent severe complications. When prescribing long-term cefepime therapy, it is important to weigh the benefits against the potential risks, including the rare but serious side effect of neutropenia.