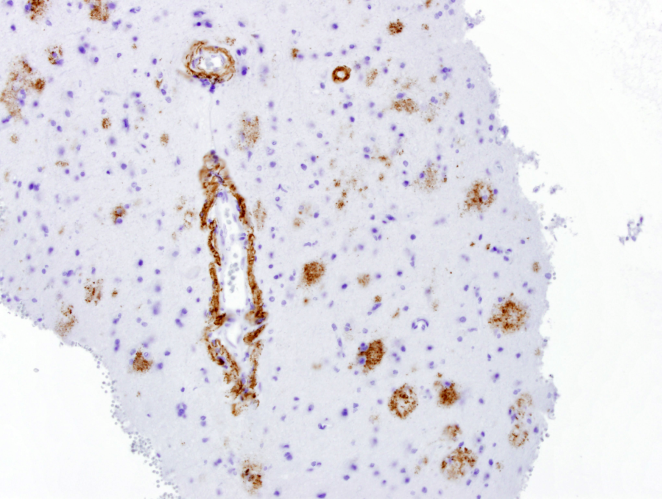
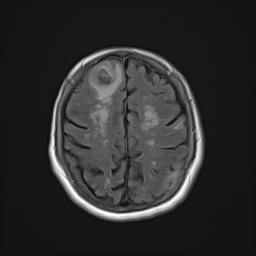
Case Presentation: We present a case of a 72 year-old independent woman on warfarin for recently-diagnosed pulmonary embolism, who was admitted to a local hospital for altered mental status. Upon presentation, a CT scan of the brain showed multiple areas of hemorrhage. The patient was transferred to our tertiary hospital for further management. An MRI of the brain was remarkable for multiple hemorrhagic ring-enhancing lesions with surrounding vasogenic edema, highly suspicious for hemorrhagic metastases versus abscesses. Over the next few days she had no signs of infection, so an exhaustive workup in an attempt to find a primary lesion was initiated. A CT chest, abdomen, and pelvis resulted in no findings suggestive of a primary lesion. A thyroid ultrasound, mammogram and PET CT (skull base to upper thigh) were also negative. Further evaluation with dermatology showed basal cell carcinoma of the nasal wall, but no evidence of melanoma. Ultimately, a brain biopsy was obtained and showed amyloid angiopathy and organized hematoma with gliosis, but no signs of neoplasm. Given high risk for recurrent intracranial bleeding, a decision was made to discontinue anticoagulation therapy and an inferior vena cava filter was placed to decrease the risk of pulmonary embolism. She was discharged on a dexamethasone taper and levetiracetam.
Discussion: Cerebral Amyloid Angiopathy (CAA) is characterized by amyloid deposition in cerebral blood vessels. Marked deposition can lead to necrosis of the vessel walls and hemorrhage. It is commonly associated with Alzheimer’s disease but most patients with hemorrhage related to CAA do not have Alzheimer’s disease. Occasionally, CAA can present as space occupying lesions, which can be challenging to differentiate from brain neoplasms. This case can be used as a reminder to keep in mind the possibility of ICH due to CAA especially in the presence of a patient on anticoagulation. It is important to remember ICH is not always associated with hypertension. As the medical field has developed more advances and pharmaceutical options for hypertensive control, the expected incidence of ICH to decrease has not followed suit. The overall incidence is actually stable, which could be secondary to oral anticoagulation associated bleeds in our aging population.
Conclusions: This case reveals an uncommon cause of intracerebral hemorrhage easily confused with CNS malignancy. Cerebral Amyloid Angiopathy is important to consider in elderly patients on anticoagulation presenting with ICH. A lack of hypertension can be a clue to diagnosing CAA induced ICH. It is very important for clinicians to consider this entity as part of the differential diagnosis for hemorrhagic lesions in the brain, particularly in the elderly population.