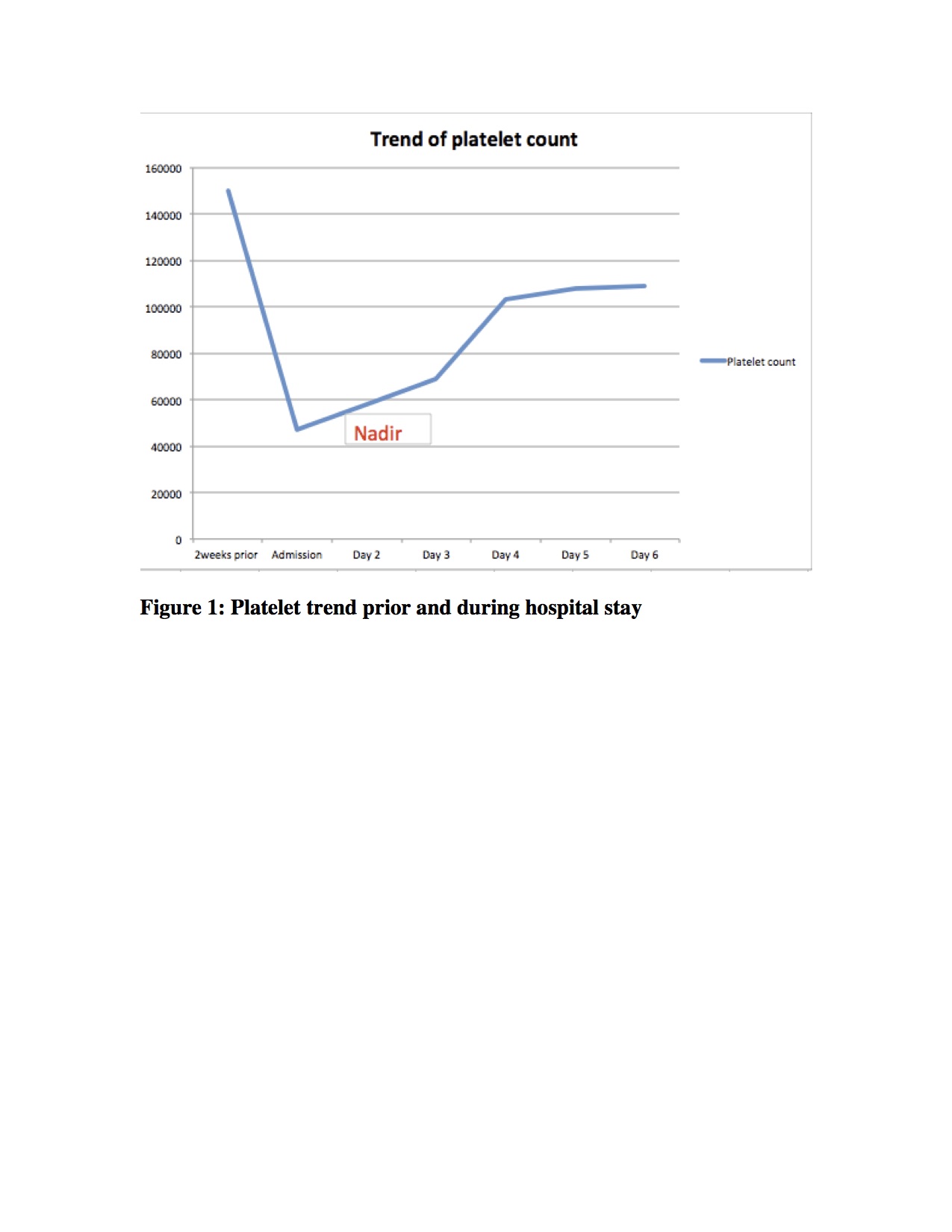
Case Presentation: A 30-year-old-woman presented to the hospital for unilateral headaches of one-week duration. Her headache was described as progressive onset, dull, radiating to the neck, and was associated with nausea and vomiting. Past medical history was notable for recent laparoscopic removal of ovarian cyst and sinusitis. Her only medication was a combined estrogen progesterone patch for contraception, and she did not report smoking. On physical exam, she was found to be tachycardic, somnolent and only oriented to self and place. No focal neurologic deficits were identified. Initial labs showed a mild neutrophilic predominant leukocytosis of 12,000/microliter and a low platelet count of 47,000/microliter. Hemolysis and coagulation studies were all within normal limits. MRI was notable for a recent thrombosis of the left transverse sinus and a 4.3cm rounded hemorrhagic parenchymal lesion in the left temporal lobe. The unusual thrombosis in the setting of unexplained thrombocytopenia raised concern for HIT (heparin induced thrombocytopenia). While there was no documented heparin administration, we hypothesized that she may have been exposed to some form of heparin in the course of her outpatient surgical procedure two weeks prior. A HIT antibody assay was performed and was positive.The contraceptive patch was removed, and the patient was started on argatroban with significant improvement of platelet count and mental status over the next few days (see figure). Further investigation from outside hospital records from her recent admission was obtained, showing no evidence of in-hospital heparin exposure. However, she subsequently reported that she had received hyperbaric ozone therapy (repeated injection of blood mixed with ozone under pressure) at a pain clinic for sinus infection 10 days before presentation, and that heparin was used in the procedure. A diagnosis of HIT was confirmed with a positive serotonin release assay and the patient was discharged on apixaban with close hematology follow up.
Discussion: The incidence of cerebral venous thrombosis (CVT) is estimated at 1.57 per 100,000 per year with a mortality rate of 12%, and a female predominance. Most common risk factors are procoagulant states (48%) and estrogen therapy (31%) [1,2]. This patient was a classic presentation of CVT, presenting with headaches, vomiting, evidence of a thrombus on imaging, and a risk factor of hormonal contraception. She met criteria for the 4T score with thrombocytopenia and recent heparin exposure from prior hyperbaric ozone therapy. This would have given her a high-risk 4T score of 6. However, at the time she was evaluated, the heparin exposure was unknown, and her presumed pre-test probability was low; she was screened for HIT based solely on clinical suspicion. Patients with intermediate or high probability score (>3) are tested for HIT antibody and, if positive, should be confirmed with a serotonin release assay. The treatment is lifelong avoidance of heparin products and use of non-heparin anticoagulation for up to 3 months [3]. Once HIT was suspected and later confirmed, our patient was started on non-heparin anticoagulation, and showed resolution of thrombocytopenia (see figure 1) and clinical improvement.
Conclusions: Although HIT is a common medical condition in internal medicine it seldom presents as CVT. An extremely high index of suspicion for HIT is needed in patients presenting with unexplained thrombosis and thrombocytopenia, as heparin exposure can be occult or unreported.