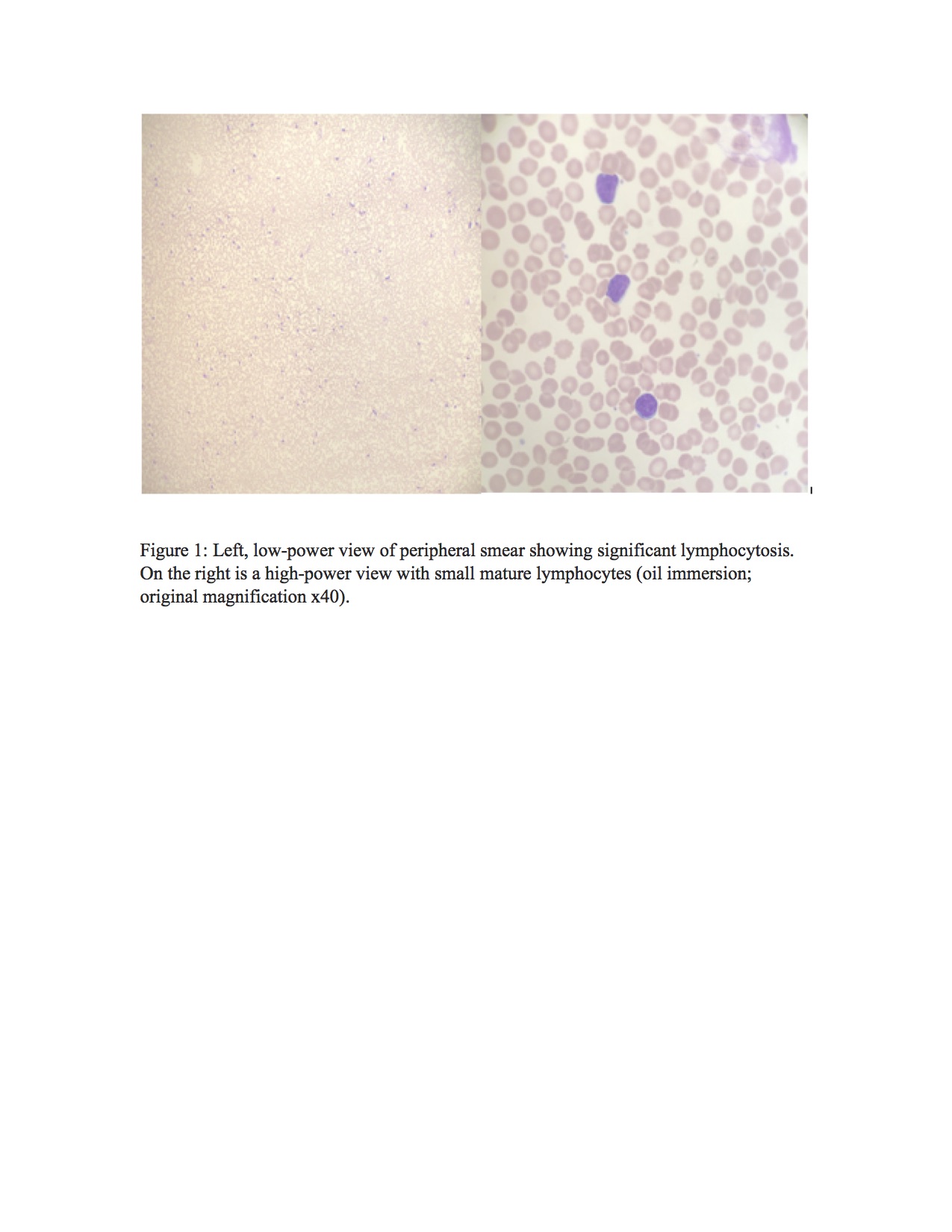
Case Presentation: An 83-year-old man presented to the hospital with eight days of shortness of breath and non-productive cough. His medical history was notable for chronic systolic heart failure, coronary artery bypass graft surgery, and hypertension. A review of systems was positive for myalgia, subjective fevers, fatigue, anorexia, and unintentional weight loss of 5 pounds in the last few months. He was found to be hypoxic requiring 4L of oxygen to keep saturation greater than 94% but otherwise afebrile and normotensive. Bilateral crackles were heard on lung examination. His rRT-PCR for SARS-CoV-2 RNA test was positive. Other labs were significant for a pre-renal acute kidney injury with a creatinine of 1.3mg/dL, elevated inflammatory markers (ferritin, lactate dehydrogenase (LDH), D-dimers), leukocytosis of 37000/µL with lymphocytic predominance at 83% (absolute lymphocyte count: 30000/µL), and 12% atypical lymphocytes. Of note, the white blood cell count obtained a year before admission was within normal limits. The peripheral smear (figure 1) showed small monotonous atypical lymphocytes with clumped chromatin. On flow cytometry, the cells were positive for CD19, CD20, CD45, lambda chain, and negative for CD5, CD23, CD25, CD200A variable FMC7, CD11c, CD103, and kappa light chain. A diagnosis of small, mature B cell lymphoma was made with differential diagnosis including atypical chronic lymphocytic leukemia (CLL), mantle cell lymphoma (MCL), and marginal zone lymphoma (MZL). The specimen was sent for cytogenetic testing to further ascertain a diagnosis. From the COVID19 pneumonia standpoint, he was started on steroids, remdesevir, and supportive care with slow but steady recovery. Hematology follow-up was arranged upon discharge with a plan to repeat peripheral smear and flow cytometry.
Discussion: Blood count abnormalities in COVID19 pneumonia have been well established and often correlate with disease severity. The most common are leukopenia (33%), thrombocytopenia, and lymphopenia (43-82%). Lymphopenia is thought to be due to direct cell lysis or cytokine-mediated destruction and atrophy of lymphatic organs. In a cohort of 1099 patients, only 5.9% presented with neutrophilic leukocytosis [1]. Others have reported lymphopenia in 76.3% of cases, and no cases of lymphocytosis [2]. Significant lymphocytosis is not a common finding in COVID19 and its presence should prompt further workup with peripheral smear and flow cytometry to differentiate clonal (malignant) versus polyclonal (reactive, infectious) causes. Malignant lymphoproliferative disorders such as small mature B cell lymphoma are characterized by a clonal population of small lymphoid cells. Subtypes including CLL, MCL, MZL, and follicular lymphoma (FL) are distinguished based on morphology, genetics, and immunophenotypic features. The chemotherapy regimen is tailored to the specific lymphoma subtype once properly diagnosed [3]. Due to the serious and novel nature of COVID19 infection, there was a tendency to attribute lymphocytosis to this, rather than evaluate it as a separate undiagnosed condition.
Conclusions: There is still a lot to discover about Covid19 infection but ongoing chronic medical conditions should always remain in mind in appropriate clinical settings. Although reactive lymphocytosis is possible in most infections it is crucial to obtain peripheral smear and flow cytometry in patients with significant lymphocytosis to rule out lymphoproliferative disorders.