Background: Internal Medicine Teaching Teams (IMTTs) aim to deliver both exceptional clinical education and efficient, high-quality patient care. However, increasing workloads and the fast pace on inpatient wards are challenging this dual objective. Our study sought to understand the tensions between education and clinical practice in IMTTs and how academic leaders are addressing these challenges.
Methods: We employed a constructivist grounded theory approach, recruiting leaders from North American academic medical centers through purposive sampling. Data collection included semi-structured individual and group interviews that we analyzed iteratively. This involved initial coding followed by preliminary theme development and, ultimately, construction of an explanatory conceptual model. We ensured rigor of our model through constant comparison and return-of-findings sessions where we presented the model back to participants for feedback. The study received Western, Johns Hopkins, and Mayo Clinic IRB exemption.
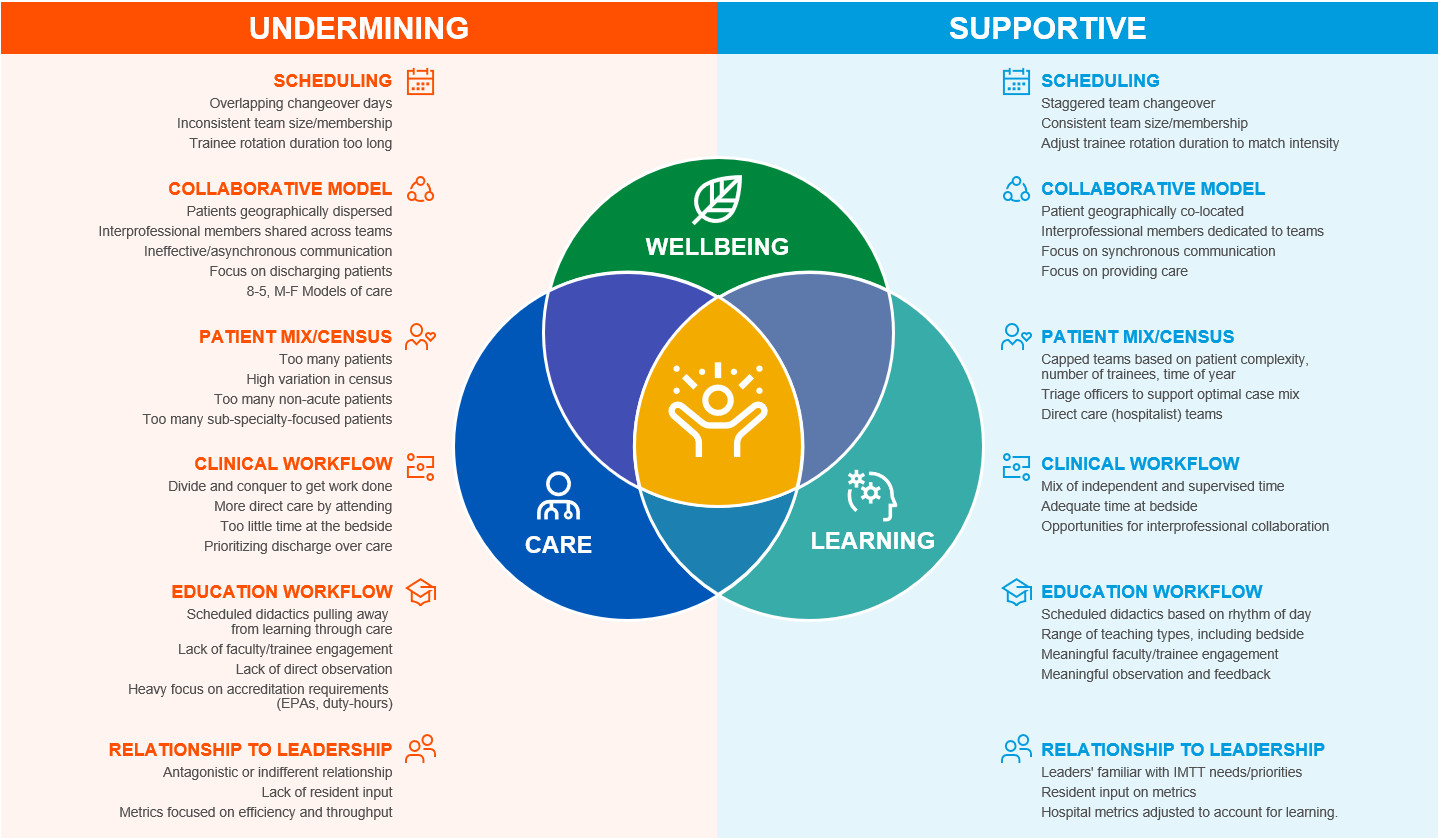
Results: We conducted 20 interviews involving 27 participants from 19 distinct training programs across the US and Canada. We developed a conceptual model focusing on three key concepts: 1) value of the IMTT rotations, 2) their challenges and their consequences, and 3) determinants of success. Participants emphasized IMTTs’ unique value in medical education, particularly its apprenticeship-style learning between students, junior residents, and senior residents, and its interprofessional approach to providing holistic care to patients with a variety of medical conditions. Challenges identified were increasing patient volumes and complexity, hospital efficiency pressures, and fragmented multidisciplinary care. These issues led to short-term dilemmas, forcing trainees to choose between providing quality care, learning, and well-being, and long-term risks like individual burnout and forming a fragile learning environment where trainees view their work as simply a job with a heavy emphasis on getting the work done and going home. Participants noted that reactionary “workarounds” to these challenges often created new and unanticipated problems. However, they identified six key elements of a successful IMTT: 1) training/attending scheduling, 2) interprofessional collaboration models, 3) patient mix/census, 4) clinical and 5) educational workflows, and 6) relationships with hospital/educational leadership. How leaders configured their IMTT structures and processes within these domains had the potential to support or undermine the delivery of high-quality care, education, and well-being.
Conclusions: The IMTT rotation, integral to medical education, is currently facing significant challenges from a changing clinical landscape. Our findings provide a conceptual model highlight key modifiable variables, offering IMTT leaders a toolset to optimize their environments, thus supporting quality care, education, and clinician well-being.