Background: Peer observation and feedback (POF) is a well-documented tool for faculty development for both medical and non-medical educators. However, in our hospital medicine division of over 150 faculty at an urban academic center, only 16 peer observations were completed in the 2022-2023 academic year as part of our division’s voluntary, formally structured peer observation program. While barriers to POF in pediatric hospital medicine have been studied, there are none defined in the literature for adult hospitalists. We aimed to explore the perceived barriers and benefits to POF that may be contributing to low participation among hospitalists.
Methods: We created a 15-question web-based survey to define current practices and attitudes of adult hospitalists toward POF, with a focus on their perceived barriers to and benefits of participation. We distributed the survey to all hospitalists (n=218) within the 3 hospital medicine divisions (including 4 main inpatient sites) in our urban academic institution.
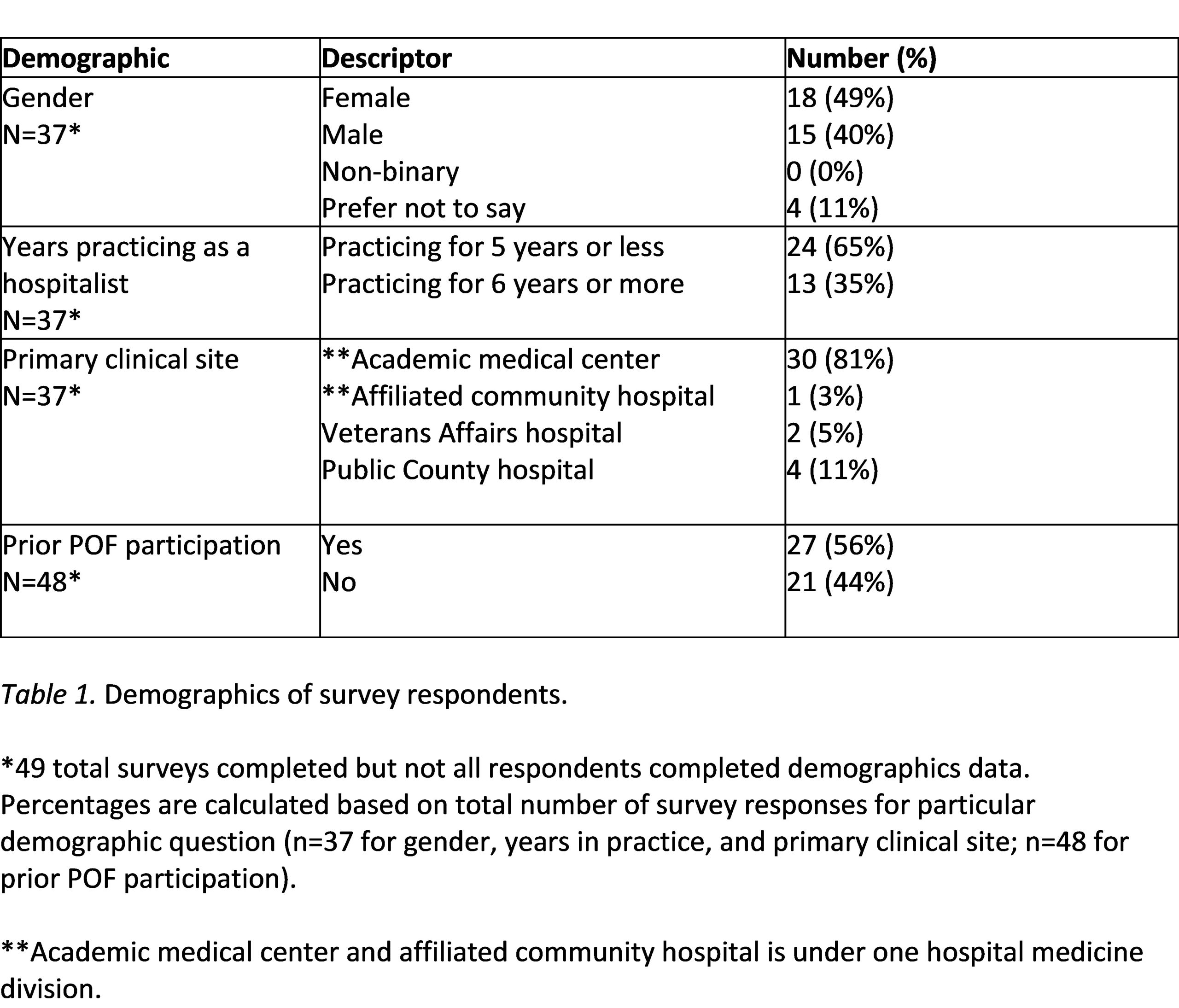
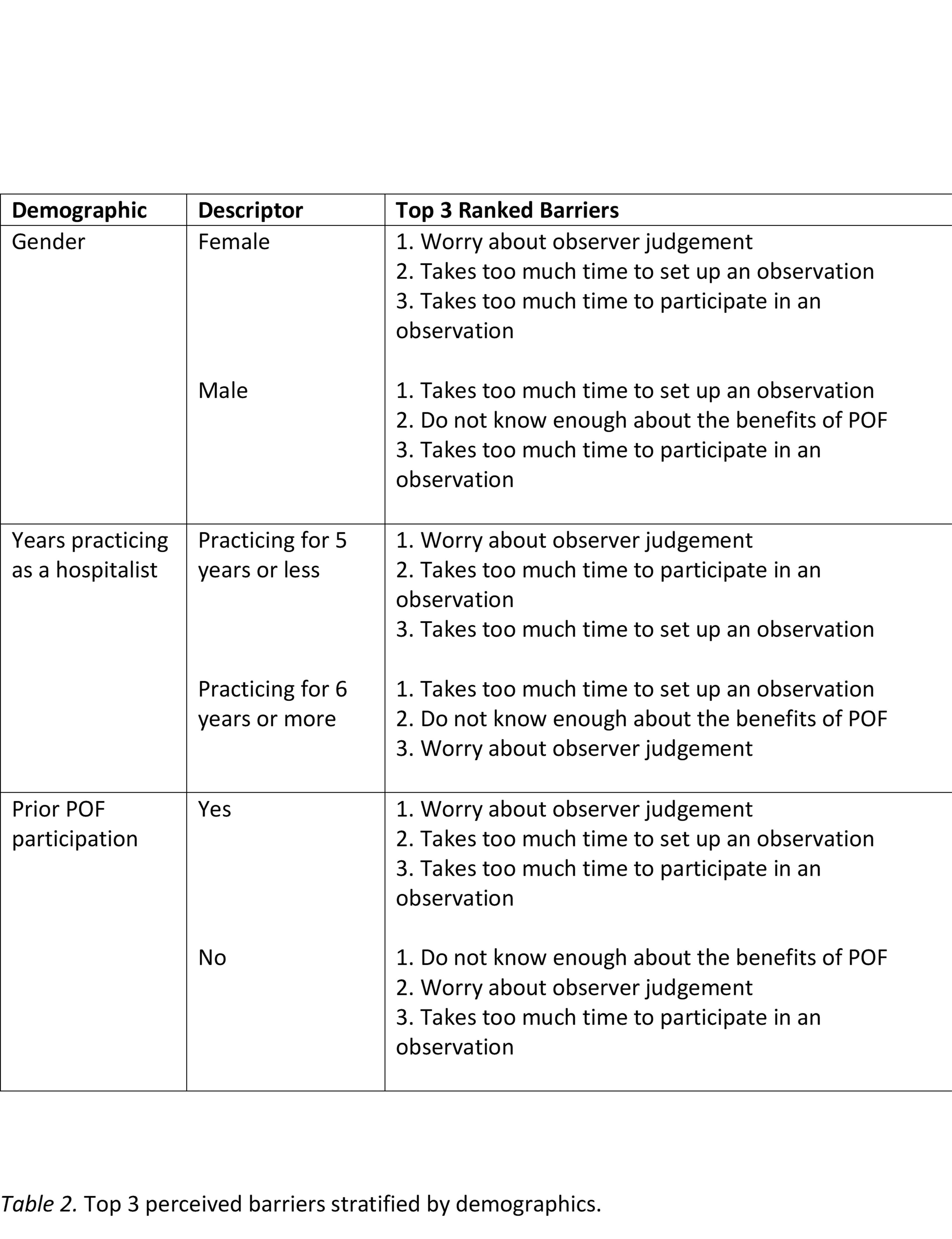
Results: There were 49 responses (22% response rate), with representation from all inpatient sites, genders, experience levels, and past POF participation (Table 1). Most respondents (95%) felt that there are professional development benefits to participating in POF, with perceived benefits in observation of multiple domains including teaching activities (95%) and clinical management (89%). Among barriers to participating in POF, the highest ranked were: 1) worrying about observer judgement 2) not knowing enough about the benefits of peer observation, and 3) taking too much time to set up an observation. Notably, stratifying by gender, years practicing as a hospitalist, and prior participation in POF revealed divergent results (Table 2). “Worry about observer judgement” was the top barrier for females, those that have been practicing hospitalists for 5 years or less, and hospitalists with prior POF participation. Meanwhile, “takes too much time to set up a POF session” was the top barrier for males and those who have been in practice for 6 years or more.
Conclusions: We successfully launched a multi-site study with adult hospitalists to better understand perspectives and barriers to POF. While most hospitalists perceive that POF will contribute to their professional development and generally desire some form of POF, there are numerous barriers that make participating in POF challenging. This study provides considerations for designing and optimizing POF programs to make them as broadly accessible and inviting as possible. Further innovations are needed to address these barriers, and subsequent studies to understand their impact.