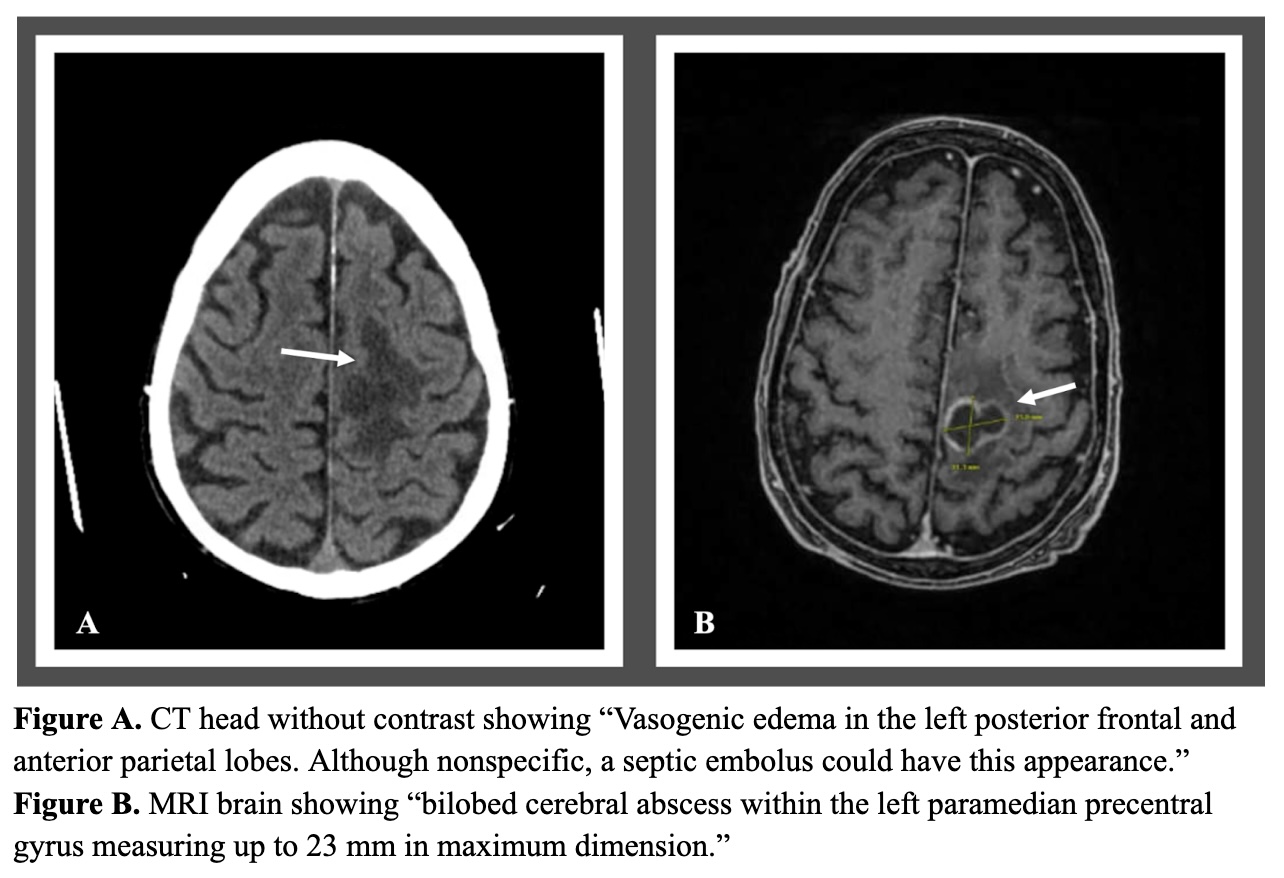
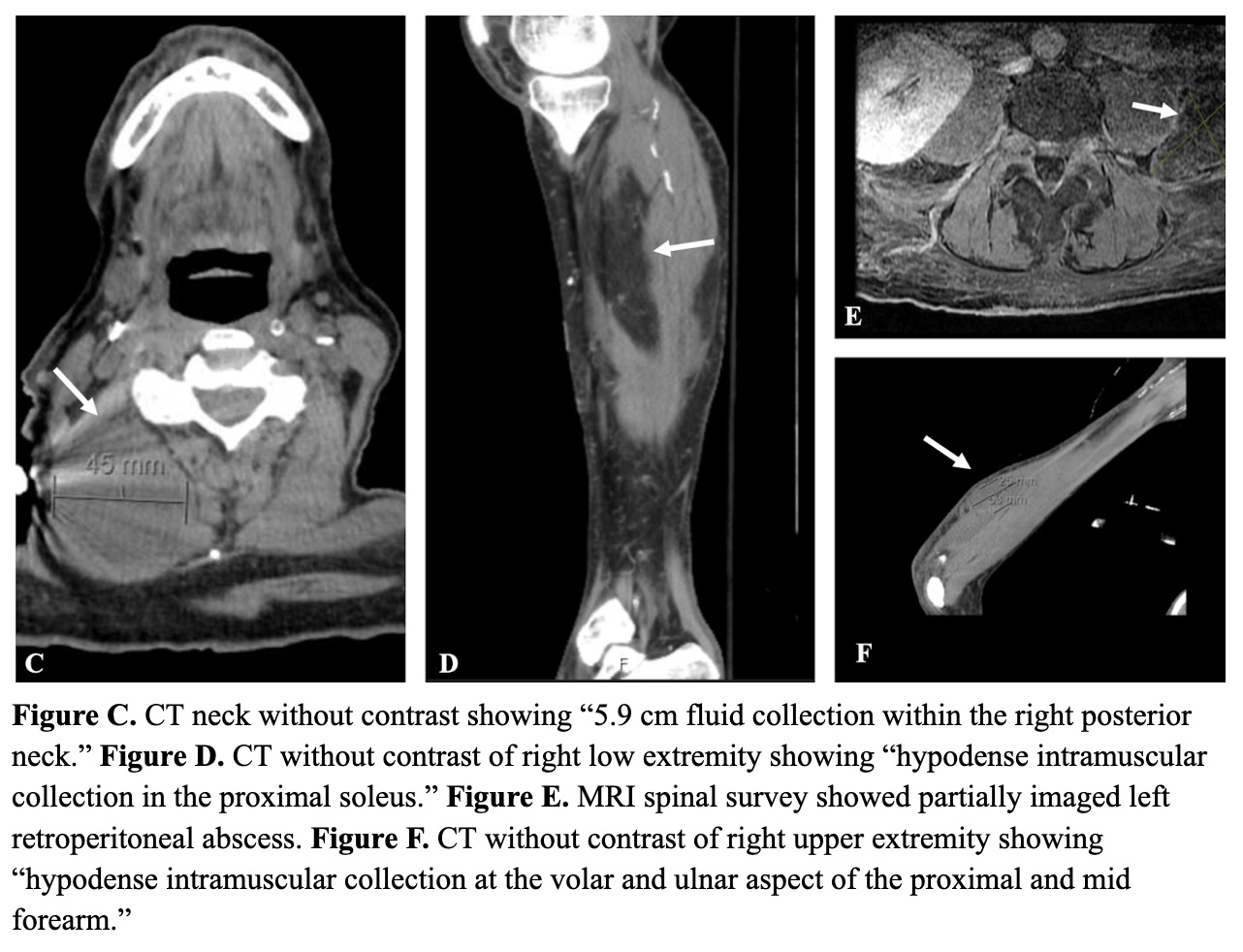
Case Presentation: A 68-year-old male with a three-year history of kidney transplantation on chronic immunosuppression presented with persistent hypotension and acute right leg pain secondary to a right lower extremity abscess. Initial comprehensive computed tomography (CT) revealed multiple additional abscesses, including neck, forearm, retroperitoneal, paravertebral and numerous pulmonary nodules. Given concerns for possible disseminated Nocardia, brain imagings were obtained several days after admission and revealed vasogenic edema associated with a 23mm cerebral abscess. Initial blood cultures were negative, so cultures of his abscesses were pursued. Two days later, gram stains from the cultures of the abscess drainage grew gram-positive rods, prompting initiation of empiric treatment for nocardiosis with imipenem, linezolid and moxifloxacin. One week later, the abscess cultures confirmed a diagnosis of disseminated nocardiosis with growth of Nocardia farcinica. Following this confirmation, sulfamethoxazole-trimethoprim was added based on sensitivities. Despite medical management, the patient continued to have persistent right lower extremity weakness with signs of possible bleeding within the brain abscess. He subsequently underwent aspiration of the brain abscess, but unfortunately his condition deteriorated post-operatively, and he passed away.
Discussion: Nocardia is an aerobic, catalase-positive, gram-positive bacillus. It is considered an opportunistic pathogen that primarily affects immunosuppressed patients, including organ transplant recipients. Pulmonary nocardiosis is the most common presentation, but Nocardia can also disseminate to other organs through continuous or hematogenous spread. Disseminated Nocardia most commonly presents within 1 to 2 years of the initial organ transplantation.All patients with suspected nocardiosis should begin empiric treatment early and obtain brain imaging if possible as the central nervous system (CNS) is the most common location of disseminated infection (44% of Nocardia cases). Intracranial abscesses are the most common abnormality on imaging. Skin and soft tissue dissemination is also possible, typically presenting with abscesses or nodular lesions. Diagnosis of nocardiosis requires microbiological culture. Treatment for Nocardia includes a prolonged course of antibiotics, such as trimethoprim-sulfamethoxazole, and surgical treatment should be considered for source control. Early detection and management are crucial; if left untreated, nocardial infection can be fatal.
Conclusions: Immunocompromised patients presenting with multi-organ abscesses and negative blood cultures should be suspected of nocardiosis. This patient with a history of kidney transplant presented with multi-organ abscesses despite negative blood cultures and was found to have disseminated nocardiosis. Nocardiosis was suspected and identified early to tailor targeted antibiotic therapy. Although brain imaging was conducted later in the hospital course, it would have been preferable to perform brain imaging earlier given his significant CNS involvement from disseminated nocardiosis. This case underscores the diagnostic and therapeutic challenges of disseminated nocardiosis, an infection associated with a high mortality rate, highlighting the importance of early recognition and intervention.