Background: While delirium may affect patients of any age, delirium initiatives have focused mostly on the elderly, as older patients are more vulnerable to developing delirium. Few studies have reported delirium in patients between 18-64 years of age, mostly restricted to patients with advanced cancer or on palliative care units. There is a lack of literature on delirium among young adults. In this study, we report the characteristics of patients 18-65 years of age, comparing those with and without delirium during their hospitalization at our academic medical center.
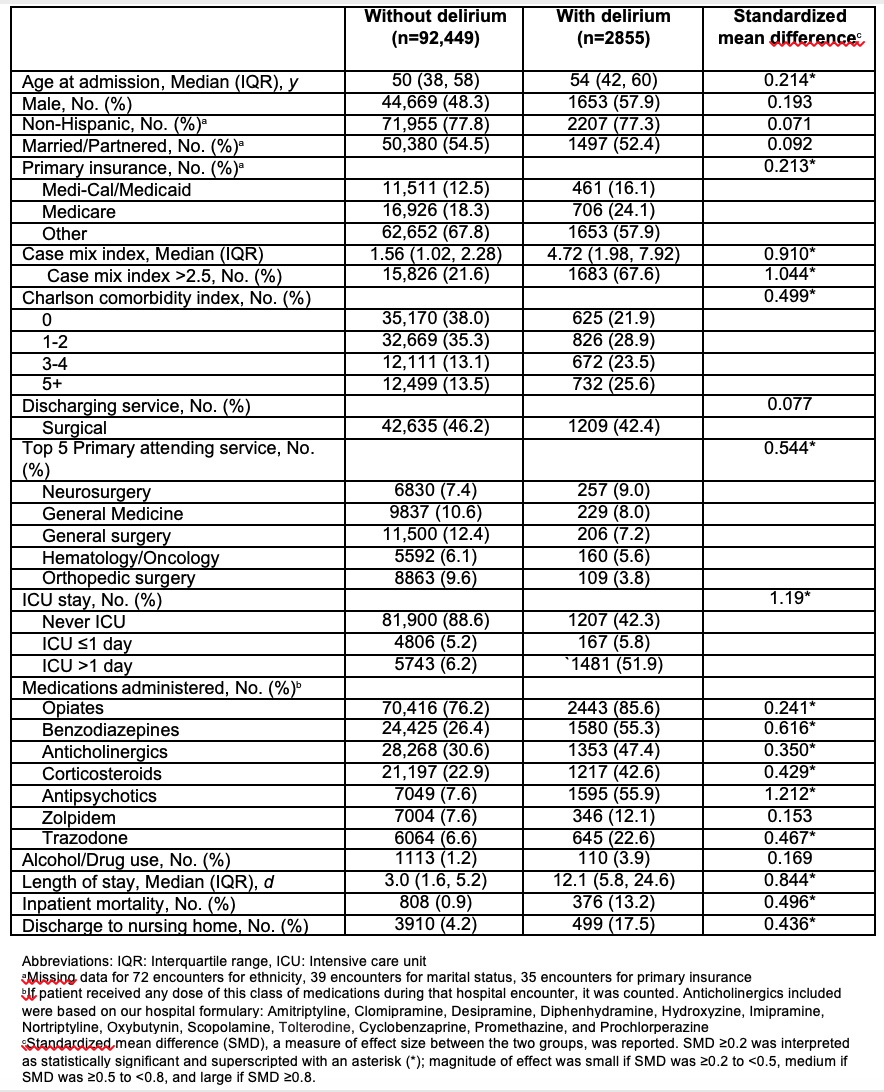
Methods: We included 95,304 patients between 18 and 65 years of age who were discharged between November 1, 2013 and January 31, 2018 from our 477-bed hospital. Delirium was identified using international classification of disease (ICD) codes (not present on admission). We conducted bivariate analysis on patients with and without delirium. Variables with standardized mean difference (SMD) ≥0.2 in the bivariate analysis were included in the multivariate model; variables were retained in the multivariate model if they had a p<0.05.
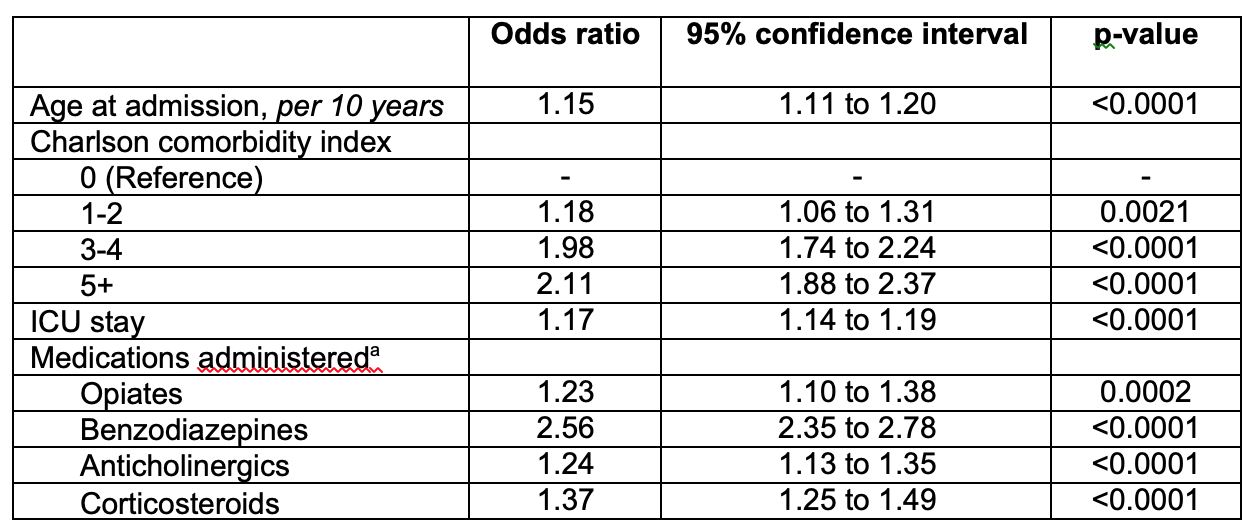
Results: 2855 (3.0%) patients between 18-64 years of age had incident delirium (compared to 5.5% patients >65 years of age). The median age of patients with delirium was 54 years. 49.1% of the patients with delirium had Charlson comorbidity score ≥3 compared to 26.6% without delirium. The median case mix index, a measure of patient acuity, was 4.72 for patients with delirium compared to 1.56 for patients without delirium. Patients with delirium were more likely to have received deliriogenic medications such as opiates (85.6% versus 76.2%), benzodiazepines (55.3% versus 26.4%), anticholinergics (47.4% versus 30.6%), and corticosteroids (42.6% versus 22.9%). 55.9% patients with delirium received antipsychotics compared to 7.6% of patients without delirium.42.4% patients with delirium never went to the intensive care unit (ICU) during their hospitalization while 51.9% were in the ICU for >1 day. Inpatient mortality was 13.2% among patients with delirium compared to 0.9% among patients without delirium. Patients with delirium were more likely to be discharged to a nursing home (17.5% versus 4.2%). The median length of stay (LOS) was 12.1 days for patients with delirium compared to 3.0 days for patients without delirium.In the multivariate analysis, the odds of delirium increased by 15% for every 10-year increase in age above 18 years (p<0.0001). The odds of delirium increased with increase in Charlson comorbidity index. The odds of delirium were higher for patients who went to the ICU during their hospital stay (OR, 1.17 [95% CI, 1.14 to 1.19], p<0.0001), or received opiates (OR, 1.23 [95% CI, 1.10 to 1.38], p=0.0002), benzodiazepines (OR, 2.56 [95% CI, 2.35 to 2.78], p<0.0001), anticholinergics (OR, 1.24 [95% CI, 1.13 to 1.35], p<0.0001), or corticosteroids (OR, 1.37 [95% CI, 1.25 to 1.49], p<0.0001).
Conclusions: Compared to patients without delirium in this age group, patients with delirium were sicker, more likely to have received deliriogenic medications, had higher mortality, longer LOS, and more discharges to nursing home. Hospitalized patients in the 18-65 year age group who are severely sick, requiring or not requiring ICU stay, may be at high risk of delirium.