Background: Health care equity, one of the six domains of high-quality health care as defined by the Institute of Medicine, will only be achieved when health care outcomes do not vary based on patient social characteristics, such as gender, race, ethnicity, geographic location, and socioeconomic status. Readmission is a significant outcome for patients and health systems, and 30-day readmission has been associated with racial disparities. However, less is known about disparities in 7-day readmissions across race and ethnicity. Previous studies have demonstrated that 7-day readmissions reflect a similar patient mix to 30-day readmissions, but that 7-day readmissions may be a better measure of hospital care. Readmissions beyond 7 days may be driven by factors beyond a hospital’s control. In the realm of health equity, studying 7-day, as opposed to 30-day readmissions, may better capture modifiable factors, diagnostic error, clinical decision making, and implicit bias from the provider.
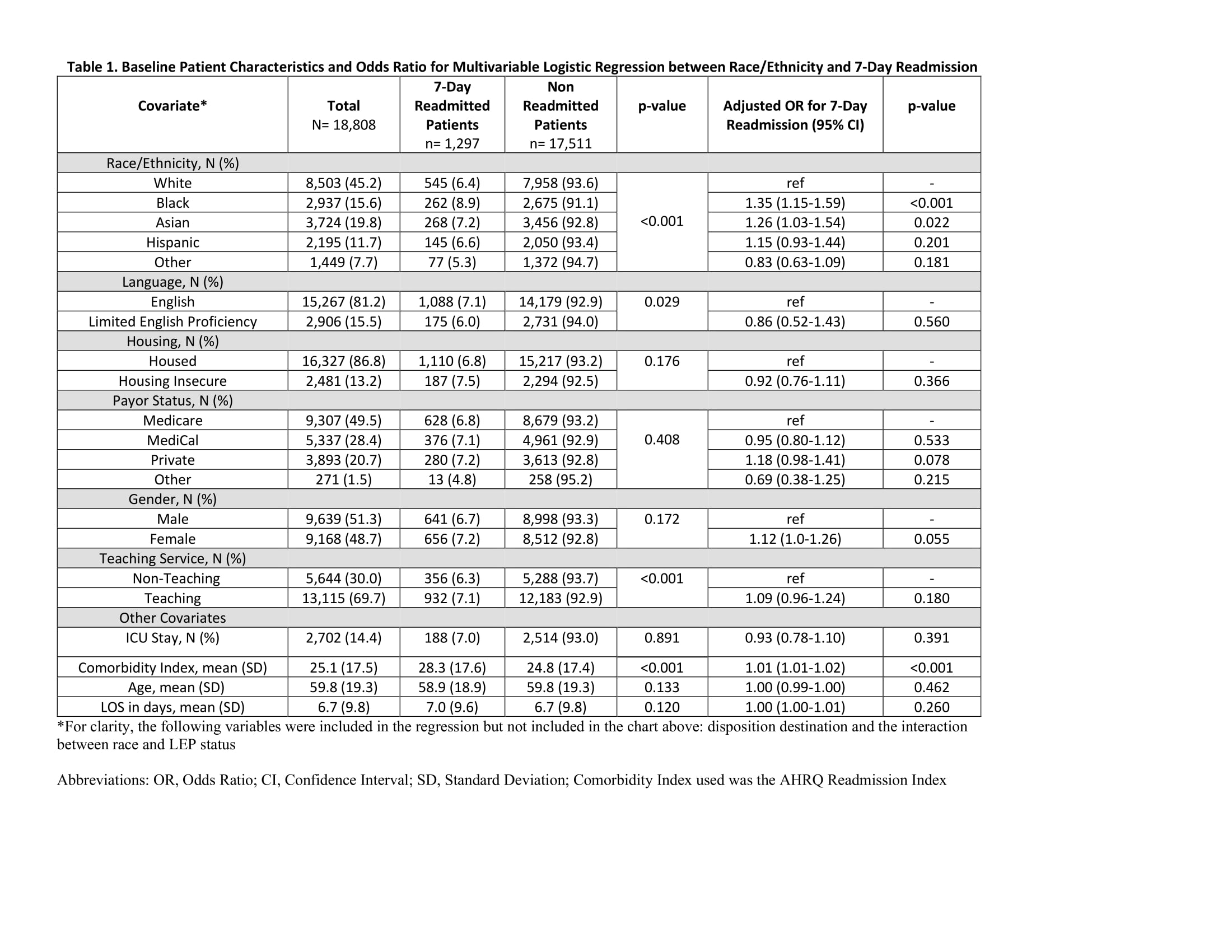
Methods: Using electronic health databases, we identified all adults discharged from the hospital medicine service between July 2016 and June 2019 from a 600-bed urban academic teaching hospital. Given the primary outcome of readmission, we excluded patients who died during hospitalization, were under observation status, or were transferred to a psychiatric facility. The primary predictor was self-reported race/ethnicity, categorized as White, Black, Hispanic, Asian, or Other/Unknown. The primary outcome was 7-day readmission back to the discharging hospital. Multivariable logistic regression was used to assess for factors associated with 7-day readmission adjusted for patient demographics (age, gender, Limited English Proficiency (LEP status), housing status, payor status), hospitalization and health system factors (including length of stay, intensive care unit management, teaching vs. hospitalist service, discharge disposition), and medical comorbidity index.
Results: We identified a total of 18,808 patients in this dataset. A total of 1,297 (6.9%) of patients were readmitted within 7 days. We found a statistically significant association between race/ethnicity and 7-day readmission. Black patients (8.9%) and Asian patients (7.2%) had a higher 7-day readmission rate compared to White patients (6.4%). Using multivariable logistic regression, controlling for confounding variables, the Odds Ratio for 7-day readmission for Black patients was 1.35 (95% CI 1.15-1.59, p <.001) and for Asian patients was 1.26 (95% CI 1.03-1.54, p = .022).
Conclusions: Black and Asian patients experienced higher rates of 7-day readmission than White patients, confirmed on adjusted analysis. Racial disparities in 7-day readmissions from hospital medicine services have not been previously characterized, but these findings align with known racial disparities in 30-day readmissions. Because 7-day readmissions may be more modifiable and impacted by factors like clinician bias, these results require further investigation into causal pathways and the development of tools to mitigate bias.