Background: Throughout the COVID-19 pandemic, the practice of intubation for hypoxemic respiratory failure secondary to presumed COVID ARDS has shifted from earlier to later intubation at our hospital. Patients are now intubated for respiratory fatigue rather than for only hypoxemia. Timing of intubation has not been associated with change in mortality based on one recent cohort study. (1) However, the morbidity risk of delayed intubation remains unknown given the prolonged requirements of very high fraction of inspired oxygen (FiO2). Hyperoxia is known to cause reactive oxygen species that lead to inflammation with potential for eventual fibrosis of the lung tissues. (2) It has also been postulated that in non-intubated patients, high respiratory drive could contribute to patient self-inflicted lung injury as patients do not breathe with lung protective low tidal volumes. (3,4) Our study examines a unique population of severely ill COVID-19 patients requiring up to 100% FiO2 by high flow nasal cannula (HFNC) with or without the addition of a non-rebreather (NRB) during their illness who did not require intubation.
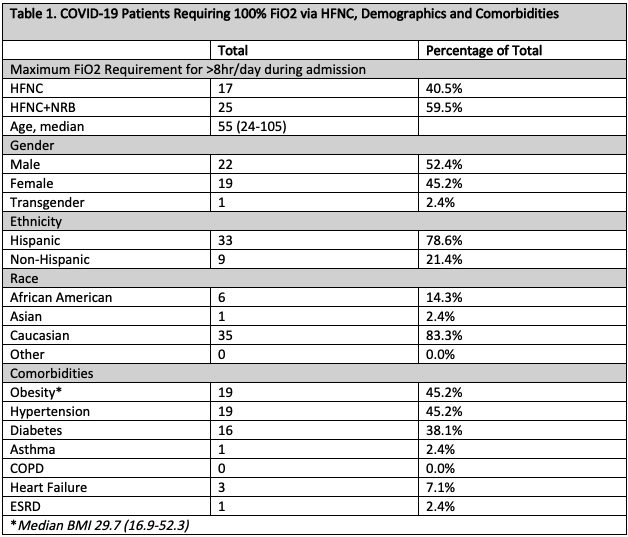
Methods: A retrospective chart review was performed for COVID-19 admissions at our 900-bed academic safety-net hospital from March 9, 2020 to September 16, 2020 who were not intubated but required up to 100% FiO2 by HFNC with or without the addition of a NRB. Patient characteristics including demographics, comorbidities, average symptom day on presentation, treatments, number of secondary infections, and average duration of 100% FiO2 were analyzed. Data was analyzed using descriptive statistics.
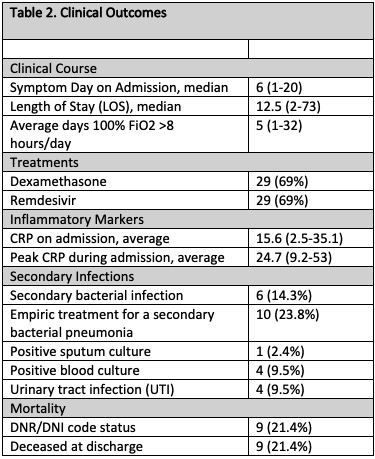
Results: Of the 42 patients evaluated, 40.5% (n=17) required HFNC 100% FiO2 and 59.5% (n=25) required HFNC+NRB for maximum respiratory support during admission. On average, these patients required 100% FiO2 for 5 days during admission. No patients were admitted to the intensive care unit. The median age was 55, and 52.4% were male. The majority were Hispanic (78.6%, n=33). The median BMI was 29.7. Diabetes, hypertension, congestive heart failure, and ESRD were present in 38.1% (n=16), 45.2% (n=19), 7.1% (n=3), and 2.4% (n=1) respectively. The median symptom day on presentation was 6 days, and the median length of stay was 12.5 days. Of patients evaluated, 69% (n=29) received Remdesivir and dexamethasone. Confirmed secondary bacterial infections were identified in 14.3% (n=6), and 23.8% (n=10) were treated empirically for a secondary bacterial pneumonia. The mortality was 21.4% (n=9), and all deceased patients were DNR/DNI at the time of death.
Conclusions: Our results highlight a unique group of patients presenting with severe COVID-19 pneumonia receiving 100% FiO2 via HFNC or HFNC+NRB for at least 8 hours per day without requiring intubation. Our patients were noted to have high incidences of obesity, diabetes, and hypertension. We identified few proven secondary bacterial infections, but the patients were treated empirically for bacterial pneumonias frequently. The average duration on 100% FiO2 of 5 days suggests a trial of HFNC with or without NRB could possibly avoid intubation in select patients. In addition, these patients did not require ICU admission at our institution which conserved limited resources. Further research is required to investigate potential adverse effects of prolonged hyperoxia in these patients.