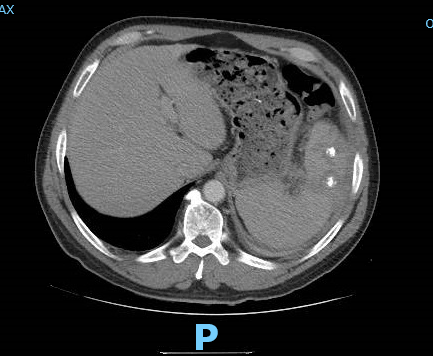
Case Presentation: A 59-year-old male with a history of Factor V Leiden and BPH presented with three weeks of worsening left flank pain accompanied by intermittent fevers and fatigue. He also endorsed a history of persistent fevers a few months ago which resolved without treatment. The patient immigrated 30 years ago from rural Italy, and last visited 2 years prior to presentation. His admission vital signs were notable for a fever of 38.6 C. His physical exam was nonfocal. His white blood cell (WBC) count was normal. ESR was elevated to 82 mm/hr and CRP was 236 mg/L. Blood cultures and urinalysis were negative. His EKG and chest x-ray were unremarkable. Contrast CT of the chest, abdomen and pelvis demonstrated splenomegaly, multiple splenic lesions with central course calcification, and multiple perisplenic collections with surrounding inflammation, the largest in the gastrosplenic region that measured 3×3 cm. Per interventional radiology, the collections were not amenable to drainage. He was empirically started on ceftriaxone and azithromycin. The patient underwent an extensive infectious work up for bacterial, fungal, and viral etiologies of splenic abscesses. TTE showed no evidence of vegetations. He also underwent a thorough rheumatologic work up which was negative. Titers for brucella IgM and IgG returned markedly elevated at 1:640. He was switched to doxycycline and rifampin and discharged home. The patient continued to have recurring fevers despite adequate antibiotic treatment with increase in splenic abscess size on repeat CT. Two months later, he underwent elective splenectomy with partial gastrectomy. Testing of splenic tissue returned positive for Brucella melitensis PCR, but tissue culture remained negative. On further history, it was revealed that the patient drank unpasteurized goat milk on his visits to Italy.
Discussion: Brucellosis is a zoonotic infection transmitted to humans from infected animals via consumption of unpasteurized milk or direct contact with infected animals. Although splenomegaly may be detected in a significant number of patients, splenic abscesses are a rare complication. Detection of calcium within the abscesses is a marker of chronic disease. In this chronic form, which we suspect in our patient, traditional diagnosis via blood or tissue culture may not be possible. A high rate of negative culture has been reported in locally reactivated disease compared to primary brucellosis. In these cases, a presumptive diagnosis can be made by means of Brucella antibody titers or detection of Brucella DNA by PCR.
Conclusions: Splenic abscesses can be a rare presentation of chronic brucellosis. Given the difficulty of isolating the organism in this chronic form, and the numerous other differentials that exist for splenic abscesses, careful history is essential in pinpointing the accurate diagnosis. While prolonged antibiotic therapy is an option, persistent symptoms may require disease eradication via splenectomy.