Background: Patients with ascites due to cirrhosis frequently have some degree of thrombocytopenia and prolongation of prothrombin time. However, major bleeding rates from paracentesis are reported to be less than 1% without use of any prophylactic blood products (plasma and/or platlets) and the mortality rate is 0.016%. Consequently, practice guidelines recommend against prophylactic transfusion of blood products prior to paracentesis but limited reports suggest that this practice persists among some proiders. The prevalence of this practice among providers caring for patients hospitalized with ascites has not been characterized. We utilized the Nationwide Inpatient Sample, a national U.S. administrative database of hospitalized patients, to assess the prevalence of the transfusion of plasma (FFP) and/or platelets on the same day as paracentesis in patients with ascites and cirrhosis.
Methods: We queried the NIS to identify hospitalized patients admitted between 2004-2012 with a primary diagnosis of ascites, spontaneous bacterial peritonitis (SBP), or hepatic encephalopathy (HE). All patients had a secondary diagnosis of cirrhosis, and patients with a primary diagnosis of HE were required to have a secondary diagnosis of ascites. All adult patients who received at least 1 paracentesis were then identified using procedure code 54.91. The prevalence of the receipt of FFP and platelets were ascertained using their respective procedure codes. Statistical analysis was performed in SAS version 9.4.
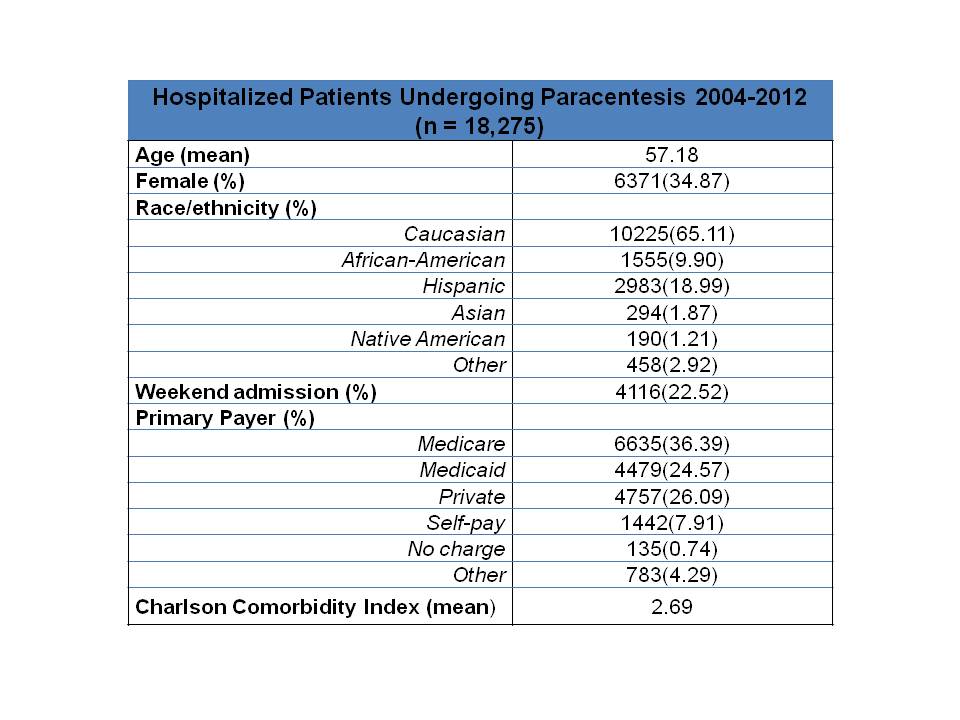
Results: 18275 eligible patients hospitalized between 2004-2012 and receiving paracentesis were identified. The average number of paracentesis performed per admission was 1.23; the maximum was 14. There were 259 (1.4%) instances of same-day platelet transfusion and paracentesis. Additionally, there were 747 (4.1%) FFP transfusions occurring on the same day as paracentesis.
Conclusions: Our study suggests that the prevalence of prophylactic transfusion of blood products is relatively low among inpatients undergoing paracentesis. However, 4.1% of paracentesis are accompanied by FFP transfusion suggesting that some providers are attempting to correct coagulation abnormalities in a prophylactic manner. Additionally, the much lower rate of platelet transfusion with paracentesis suggests that providers are less apt to prophylactically transfuse platelets compared to FFP. Prior studies have reported no increased bleeding complications in patients with a mild to moderate coagulopathy undergoing paracentesis suggesting that paracentesis is safe even in the presence of abnormal laboratory markers of hemostasis. Hence, the potential for unnecessary adverse outcomes (i.e. serious transfusion reactions) in the setting of unnecessary blood product transfusions must be considered. Additionally, the additional cost of unnecessary platelet and FFP transfusions is significant. The main limitation of this study is the inability to determine with certainty whether the concomitant transfusion of blood products and paracentesis represents prophylactic use of blood products or a response to post-paracentesis bleeding. However, the much lower reported rate of bleeding associated with paracentesis suggests that these events represent prophylactic use of blood products. An additional limitation of the administrative database used in this analysis is that non-operative, minor procedures such as transfusion of blood products may be undercoded resulting in an underestimation of our primary outcome.