Background:
Most patients who undergo hip surgery are elderly with significant comorbidities. Postoperative infection and mortality are potentially preventable complications. As with cardiac risk stratification, infection and mortality risk stratification may be possible. This study sought to identify factors associated with postoperative infection and 30‐day mortality.
Methods:
The study was a retrospective chart review of patients who underwent hip surgery between 2000 and 2001 at the Mayo Clinic, Rochester, Minnesota, a tertiary referral center, and were seen in consultation by the inpatient internal medicine service. Abstractors collected the following information: glucose concentration at admission, preoperatively, and postoperatively for 24 hours; emergency versus elective surgery; comorbid conditions used to calculate the Charlson comorbidity index; incidence of intraoperative systolic blood pressure less than 120 and less than 80; incidence, timing, and location of infection; body mass index (BMI); length of hospital stay; and 30‐day hospital mortality. Olmsted County database was searched for deaths within 30 days. Infection was defined as having been diagnosed by the treatment team and having had antibiotics initiated to treat that infection before discharge. Administration of steroids pre‐ or postoperatively was recorded, as was administration of preoperative antibiotics not for surgical prophylaxis. All patients received antibiotics for surgical prophylaxis. One patient had emergency surgery, defined as threatened loss of life without immediate operation. the primary end point was infection before hospital discharge. Thirty‐day mortality was a secondary end point. Multivariant analysis was performed to assess factors associated with postoperative infection and/or all‐cause mortality.
Results:
Three hundred and ninety‐four patients were studied, of whom 80% were white and 75% were female. Mean age was 83 years (64‐106 years), and mean length of hospital stay (LOS) was 10.7 days (2‐122 days, median 8 days).
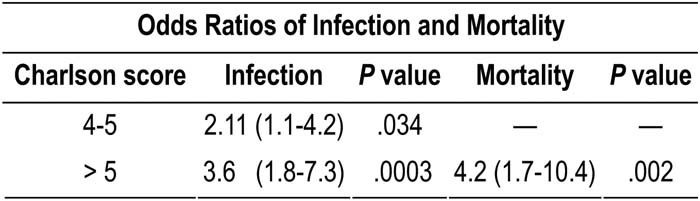
Seventy‐six patients (19.3%) developed infections; almost half (48%) were urinary tract infections, and 85% were diagnosed by postoperative day 8. Thirty‐one patients (7.9%) died within 30 days postoperatively. The Charlson index score ranged from 0 to 16. Multivariant analysis results are shown in the table.
Conclusions:
Although known as a validated prognostic tool for 1‐year mortality, the Charlson morbidity index score was independently associated with postoperative infection and 30‐day mortality in elderly hip surgery patients. Application of this tool may help to identify patients at risk, allowing closer observation of or changes in the process of perioperative care.
Author Disclosure:
L. L. Kirkland, None.