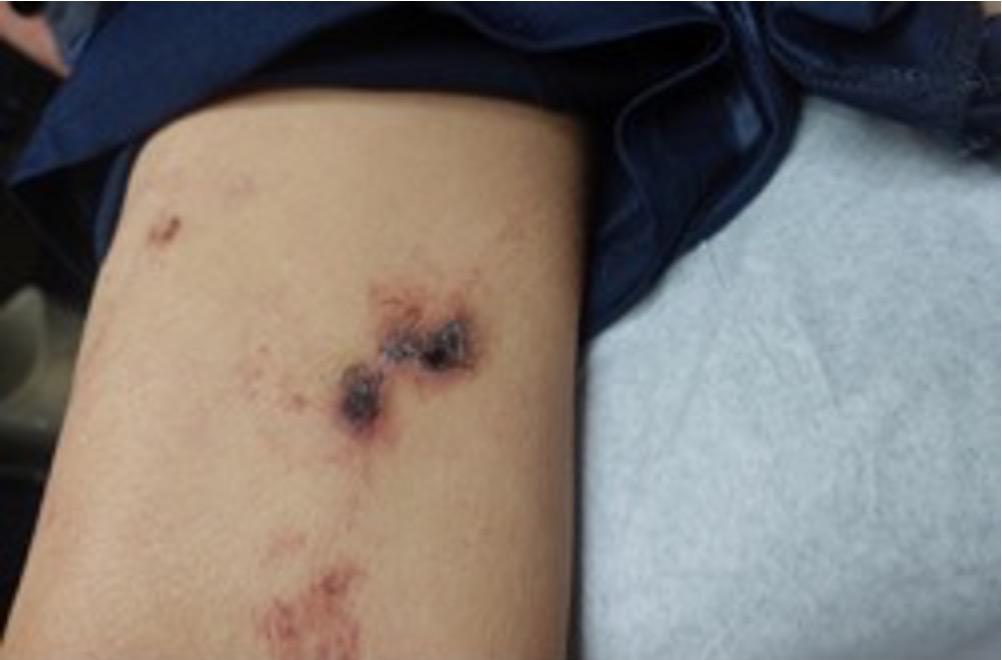
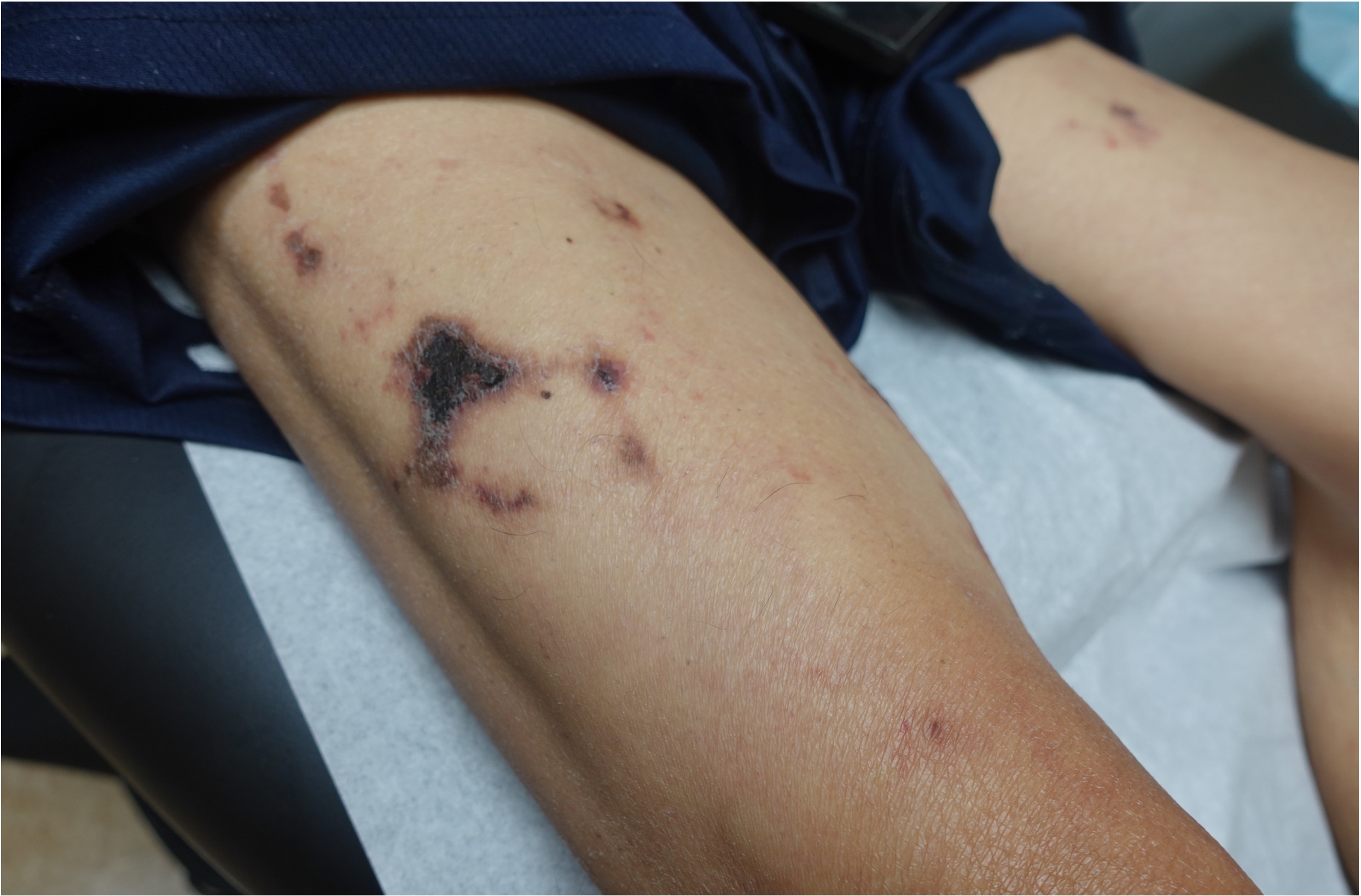
Case Presentation: A 56-year-old male with severe diffuse atherosclerotic disease presented to primary care clinic following several hospitalizations requiring vascular intervention. Physical exam revealed multiple large (10 cm), scattered, painful plaques with central necrosis and erythematous borders on the bilateral upper thighs. Cutaneous biopsy showed ulceration with cholesterol emboli confirming CES. Upon diagnosis, a retrospective chart review revealed early signs of CES not previously identified. Two months prior to his clinic visit, the patient was admitted for left femoral endarterectomy with bypass. Following the procedure, his creatine rose to 1.5mg/dL from his baseline of 1.0 mg/dL. A transient eosinophilia and leukocytosis were also noted on labs. His renal function continued to decline over the next few weeks to and peaked at a creatinine of 3.3 mg/dL. The bypass procedure is suspected to have precipitated the development of CES. His condition was likely exacerbated by the need for heparin due to a provoked DVT. He was subsequently admitted two days later with an NSTEMI requiring cardiac catheterization and further anti-coagulation with heparin. While myocardial infarction is a recognized complication of CES, he had severe multi-vessel disease, which may have preceded the embolic event. However, the repeat use of anticoagulation and a second vascular procedure likely worsened his condition.
Discussion: Cholesterol Embolization Syndrome (CES) typically arises following vascular intervention. The most common manifestations include renal impairment and cutaneous lesions, such as livedo reticularis, gangrene, and blue toe syndrome. Skin findings typically involve distal extremities, but proximal lesions have been documented as seen in this case. Evidence of end-organ damage manifests as slowly progressive dysfunction occurring weeks to months after the triggering event, distinguishing it from thromboembolism from aortic plaque, which has a rapid onset. Additional supportive findings include transient eosinophilia, leukocytosis, and elevated CRP. Skin biopsy has the highest sensitivity to confirm the diagnosis, however clinical diagnosis can be made based on characteristic features occurring after vascular intervention. As changes may be subtle, a thorough physical exam should be completed when CES is suspected. Use of anticoagulation has been shown to worsen outcomes in CES and should be avoided when possible. High-dose statin therapy offers anti-inflammatory effects and may improve plaque stability but does not reverse any damage. Optimizing comorbid conditions contributing to atherosclerotic disease is recommended as additional management. In summary, CES is a complex condition that necessitates a high index of suspicion for diagnosis due to its non-specific symptoms. Early recognition and appropriate management are pivotal in preventing serious complications and enhancing patient outcomes.
Conclusions: Cholesterol Embolization Syndrome (CES) is a rare condition caused by cholesterol crystal emboli settling in distal arteries resulting in progressive end-organ damage. Due to the indolent course, it frequently goes unrecognized. We present a case of CES that was diagnosed retrospectively, one month after the inciting event. We hope to highlight key points that can lead to an earlier diagnosis especially in patients with a more proximal dermatologic manifestation of CES.