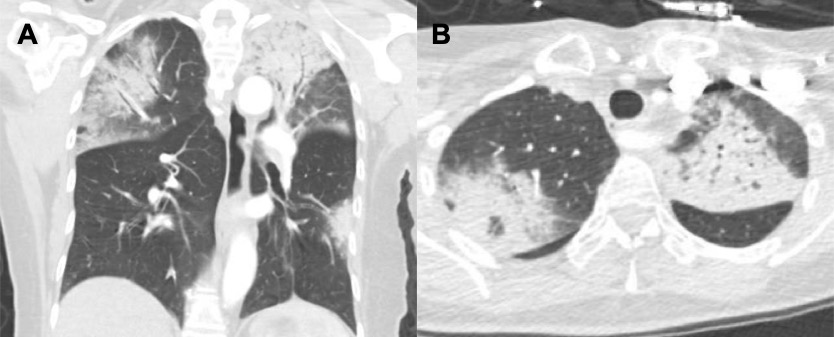
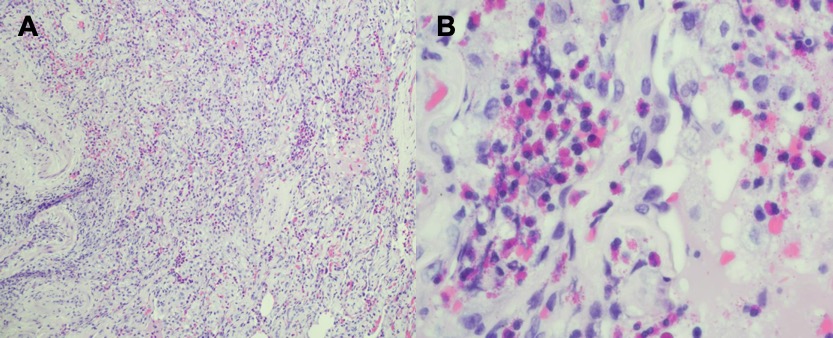
Case Presentation: We present the case of a 62-year-old female with a past medical history of breast cancer diagnosed one-year prior status post lumpectomy, adjuvant radiation, and letrozole, who presented to the hospital with a 1.5 month history of cough, night sweats, fevers, and weight loss. She reported the cough was initially productive of yellow sputum, and then became pale yellow, but denied hemoptysis. She saw her outpatient Pulmonologist during this time and was started on systemic steroids. She reported intermittent improvement in her symptoms, however after the steroid course was completed her symptoms returned. For 3 weeks preceding her hospitalization, she stopped taking any medications, and was planned to undergo outpatient PET scan. The PET scan showed FDG avid nodules with mediastinal lymphadenopathy. She was scheduled for outpatient bronchoscopy with bronchoalveolar lavage (BAL) and transbronchial biopsy, however, she was admitted from Pulmonary clinic for worsening shortness of breath and hypoxic respiratory failure. On arrival to the Emergency Department she was afebrile, heart rate 92 bpm and BP 111/75 mmHg. She was hypoxic on room air to 86% with a rate of 24 breaths per minute and was placed on 2 liters nasal cannula. Computed tomography of the chest revealed multi-lobar pulmonary consolidations with peripheral predominance that were increased from prior (Figure 1). Lab studies revealed: WBC 10.1 K/uL with normal differential, PLT 394 K/uL, CRP 89 mg/L, ESR 118 mm/hr, procalcitonin 0.05 ng/mL, undetectable Fungitell level, negative serologies for endemic mycoses, and negative autoimmune workup including anti-nuclear antibody (ANA), rheumatoid factor (RF), mitochondrial antibody (AMA), double-stranded DNA, cytoplasmic-ANCA, perinuclear-ANCA and scleroderma antibodies. Given concern for an organizing pneumonia, she underwent Video Assisted Thoracoscopic Surgery (VATS) with Thoracic surgery. Pathology revealed eosinophilic pneumonia with organization (Figure 2). The gram stain and acid fast bacilli were negative by smear. She was treated with corticosteroids with improvement in her symptoms.
Discussion: Chronic eosinophilic pneumonia (CEP) is a rare pulmonary disorder notable for the deposition of eosinophils in the pulmonary interstitium and alveoli. An association with CEP and radiation to the chest, particularly in patients with history of breast cancer, has been described.1 In CEP, nonspecific symptoms such as cough, night sweats and weight loss are often subacute to chronic before presenting for medical evaluation.2,3 Parenchymal disease is often localized in the periphery, noting a ‘photonegative’ pattern of pulmonary edema on imaging.2 The majority of patients display a peripheral blood eosinophilia and eosinophilic predominant BAL.2-4 Interestingly, we present a case of CEP without peripheral blood eosinophilia. The decision was made to pursue surgical biopsy which revealed characteristic histopathology for CEP with eosinophils in the interstitium and alveoli with organization. The mainstay of treatment is corticosteroids which our patient was successfully treated with.2-4
Conclusions: CEP is a rare diagnosis that can often be made without need for surgical biopsy based on clinical symptoms, characteristic chest imaging and eosinophilia in blood or BAL.An association of CEP and patients who have received prior chest radiation has been described.Organizing pneumonia is a commonly associated finding in surgical biopsies of patients with CEP.