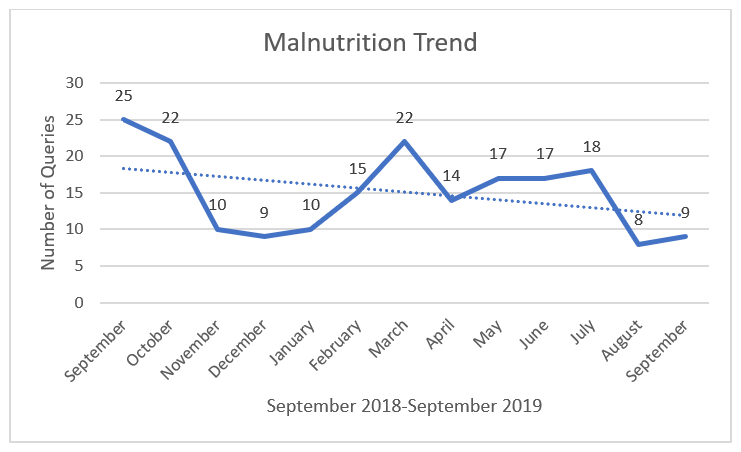
Background: Anywhere from 20-50% of all hospitalized adult patients are impacted by malnourishment on admission. Although malnutrition has a worldwide impact on patient outcomes, it is frequently under documented. This proves detrimental to patient outcomes as the average length of stay is 1.5 times greater than those not affected by malnutrition. This is further exemplified through the three times greater mortality rate at one year from discharge of malnourished patients. Malnutrition can complicate patient outcomes by increasing length of stay, infection rates, readmission rates, as well as treatment costs. By improving documentation for malnutrition, we have the potential to improve patient outcomes. Malnutrition can be a predictor for many other outcomes, and by documenting the predictor early we have an opportunity to act upon potential complications and improve patient outcomes.At Stanford Hospital, Malnutrition was frequently the number one queried item in the medicine division of the hospital. Malnutrition was queried an average of 18-20 times over the past few years, which is quite high for internal medicine. Given that malnutrition is a complex diagnosis requiring multifaceted care, we have implemented a novel solution of the group note to improve documentation. We believe that integrating the available expertise of our care extended the care team like the registered dieticians into a team note, will allow our physicians to make the diagnosis more confidently, more frequently, and more efficiently. By reducing the number of missed malnutrition diagnoses we should be able to reduce our query rate.
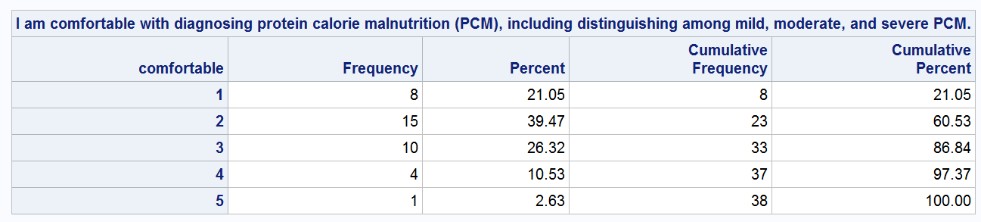
Methods: We created an intervention that improves nutritional assessment and captures malnutrition-based diagnoses in an inpatient setting.The study was conducted at the inpatient medicine setting of a tertiary academic medical center. A survey was conducted to understand the comfort and confidence of physicians in diagnosing malnutrition. A macros was set up within a physician’s note that autopopulates from dietician’s note (group note). We combine the results of this group note with that of the physician survey. This measures the physician’s comfort in diagnosing malnutrition and utilizing the dietician in making the diagnosis. We use a test of proportion to compare and contrast the query rate before and after the intervention.
Results: Our group note improves malnutrition documentation. Malnutrition was frequently the number one queried at high average of 18-20 times over the past few years. There has been a 55% drop in the number of malnutrition queries for August (8) and September (9) compared to the numbers from three (3) previous months: July (18), June (18), May (17). More than 92% of those surveyed (60% of the new interns) reported using the new progress note template (group note). More than 86% of responders indicated average or below average comfort in distinguishing between the various malnutrition categories
Conclusions: Physicians can partner with dieticians to make the malnutrition diagnosis. With more data in the following months, we will likely be able to show significance for the group note intervention. The wide-spread adoption of the group note can streamline our documentation process. Our intervention is replicable within other divisions and can become a scalable solution improving malnutrition diagnosis at other hospitals.