Background: Collaboration is essential to providing high quality care. Clinicians on primary medical services frequently consult specialists, yet little is known about the quality of collaboration between services. In our 800-bed teaching hospital, 58% of patients on general medicine units in 2017 had at least 1 consultant team, with the average patient receiving 4.8 consults. We formed an interdisciplinary group of primary medical service clinicians and specialist consultants to improve collaboration between teams delivering care in the hospital. Our aims were three-fold: 1) determine primary clinicians’ and consultants’ ratings of the quality of collaboration, 2) identify barriers to proper collaboration, and 3) to develop targeted improvements, as well as an incentive program to promote collaboration. Herein, we report results from aims 1 and 2.
Methods: To assess satisfaction with collaboration amongst primary clinicians and consultants, we surveyed both groups and asked them to rate the quality of collaboration experienced with other services. Primary clinicians surveyed included hospitalists on general medicine units and residents on the general medicine teaching service. We also surveyed the 20 most consulted services based on data from our healthcare system data warehouse. Participants included attending physicians, fellows, residents, physician assistants and nurse practitioners working on a primary service or on one of the included consulting services for the two months prior to the survey. Respondents were asked to rate the quality of collaboration with other services using a 5-point ordinal response scale and answer multiple choice and free-form questions about current practices, barriers to collaboration, and preferences in regards to consultation.
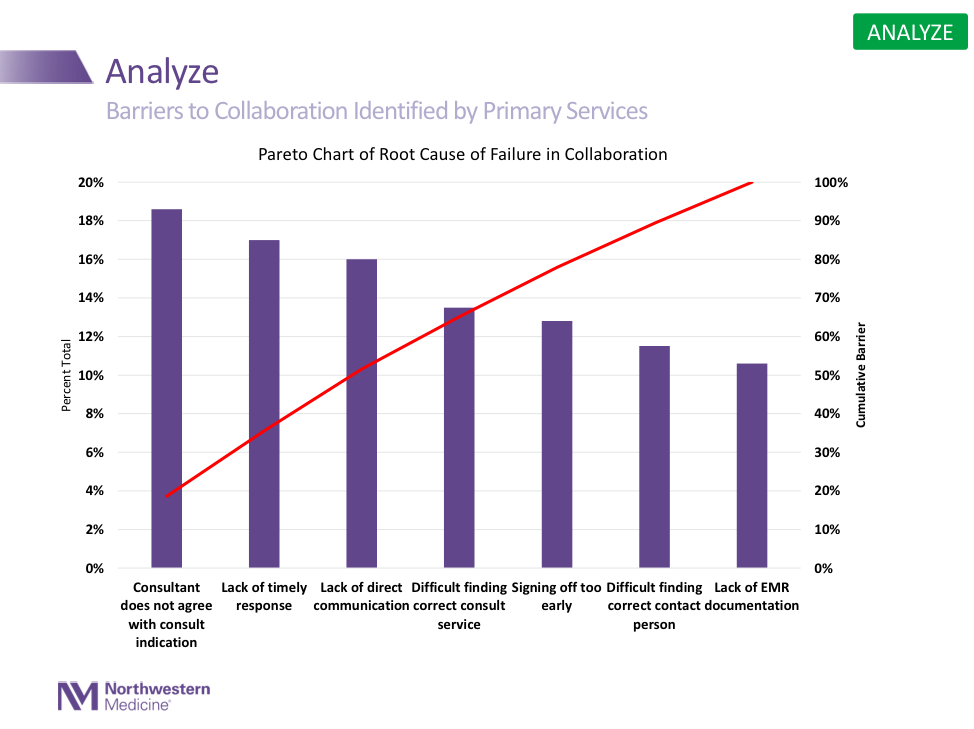
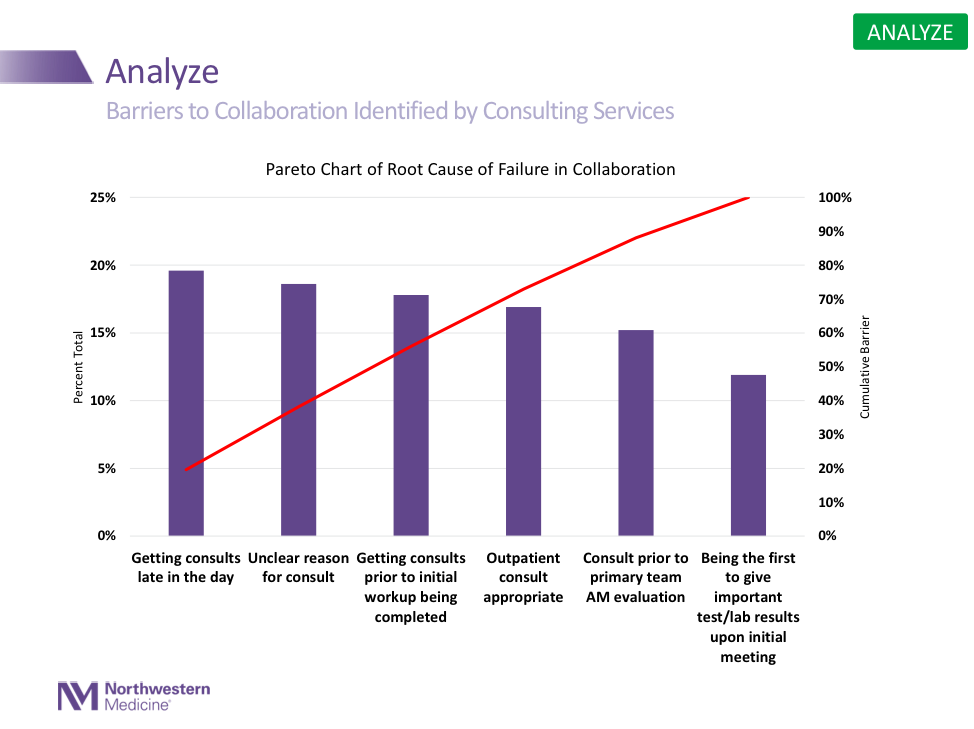
Results: In total, 92 of 155 primary clinicians (59%) and 199 of 391 consultants (51%) completed the survey. Overall, 51% of primary clinicians rated the quality of collaboration with consultants as high or very high, with a range of 18% to 86%. For consultants, 50% rated quality of collaboration with primary clinicians as high or very high with no significant difference between hospitalist service and resident teaching service. Primary clinicians gave higher mean ratings to medicine subspecialties (67%) compared to nonmedical subspecialties (30%). The main barriers to satisfactory collaboration, as assessed by primary clinicians, included lack of timely response, lack of direct communication and disagreement with reason for consult. Consultants’ top barriers for collaboration included unclear reason for consult, receiving consults prior to initial workup, and receiving consults late in the day.
Conclusions: Measurement is an essential first step to providing a deeper understanding of performance and barriers related to collaboration. We found variation in primary clinicians’ perceptions of collaboration consulting services. The variation in perceptions and a review of free form comments, has helped us identify specific services and interventions to improve collaboration. Further research is needed to determine the effect of these interventions to improve collaboration between primary medical services and specialist consultant services.