Background: Diagnostic errors are common and associated with high patient morbidity and mortality. Cognitive- and system-factors are known contributors to such errors. Diagnostic checklists that target cognitive and behavioral aspects have been suggested as potential ways to reduce diagnostic error. However, little is known about the content of these checklists and their approaches.
Methods: We systematically searched PubMed, EMBASE, Scopus and Web of Science from inception to April 30, 2019. Two authors independently reviewed and selected studies that included an explicit checklist or step-based approach to diagnosis. Studies where checklists were used to screen for or diagnose a single disease or condition, or process-based checklists (e.g. procedural or surgical time-out checklists) were excluded. To categorize checklist elements and facilitate comparison, checklist contents were analyzed using the Systems Engineering Initiative for Patient Safety (SEIPS) 2.0 human factors framework. Additionally, cognitive components of extracted checklists were categorized based on whether they included: a list of differential diagnosis, a process to narrow down the differential, urgent medical conditions, rare medical conditions, physical exam or tests, and common diagnostic pitfalls.
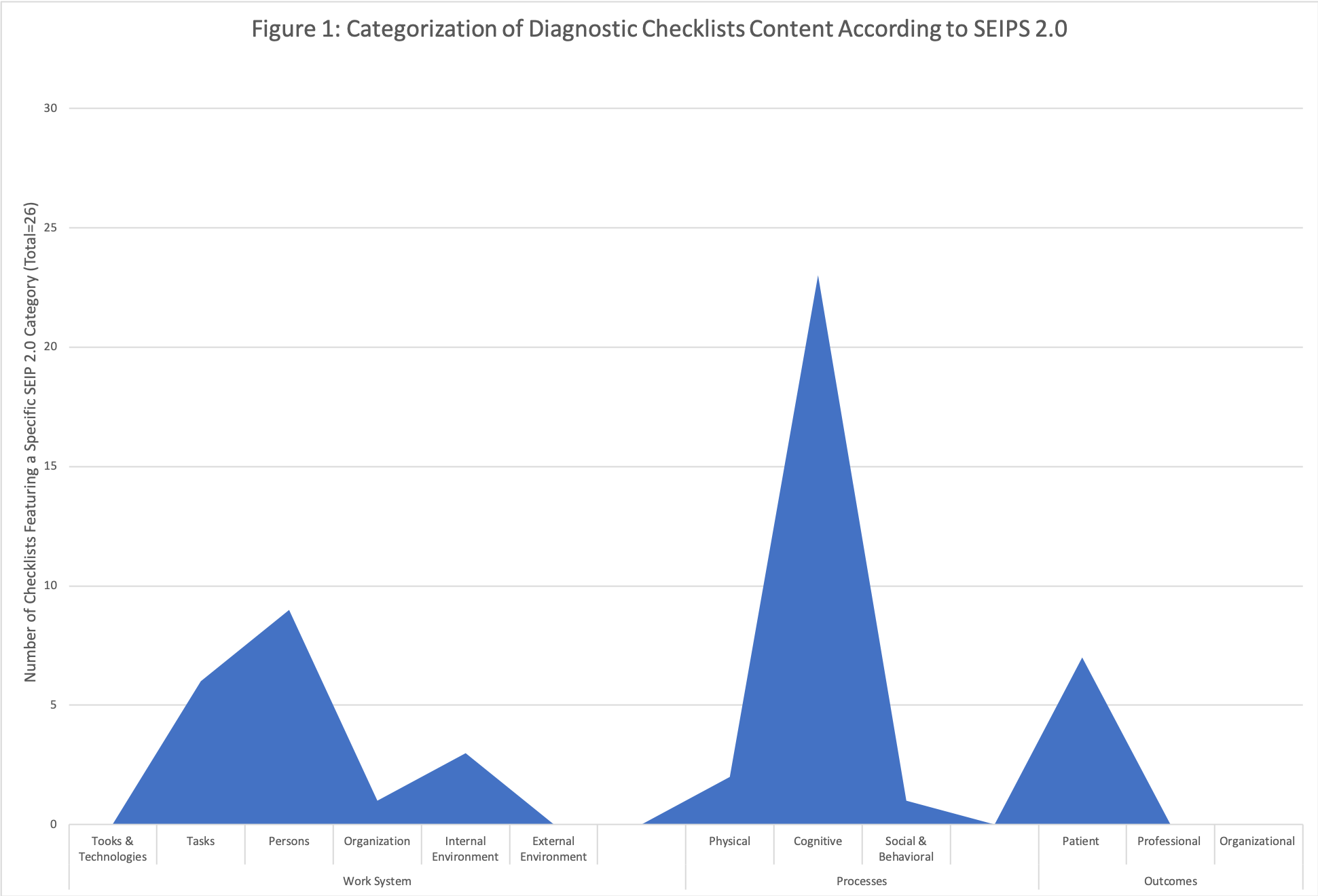
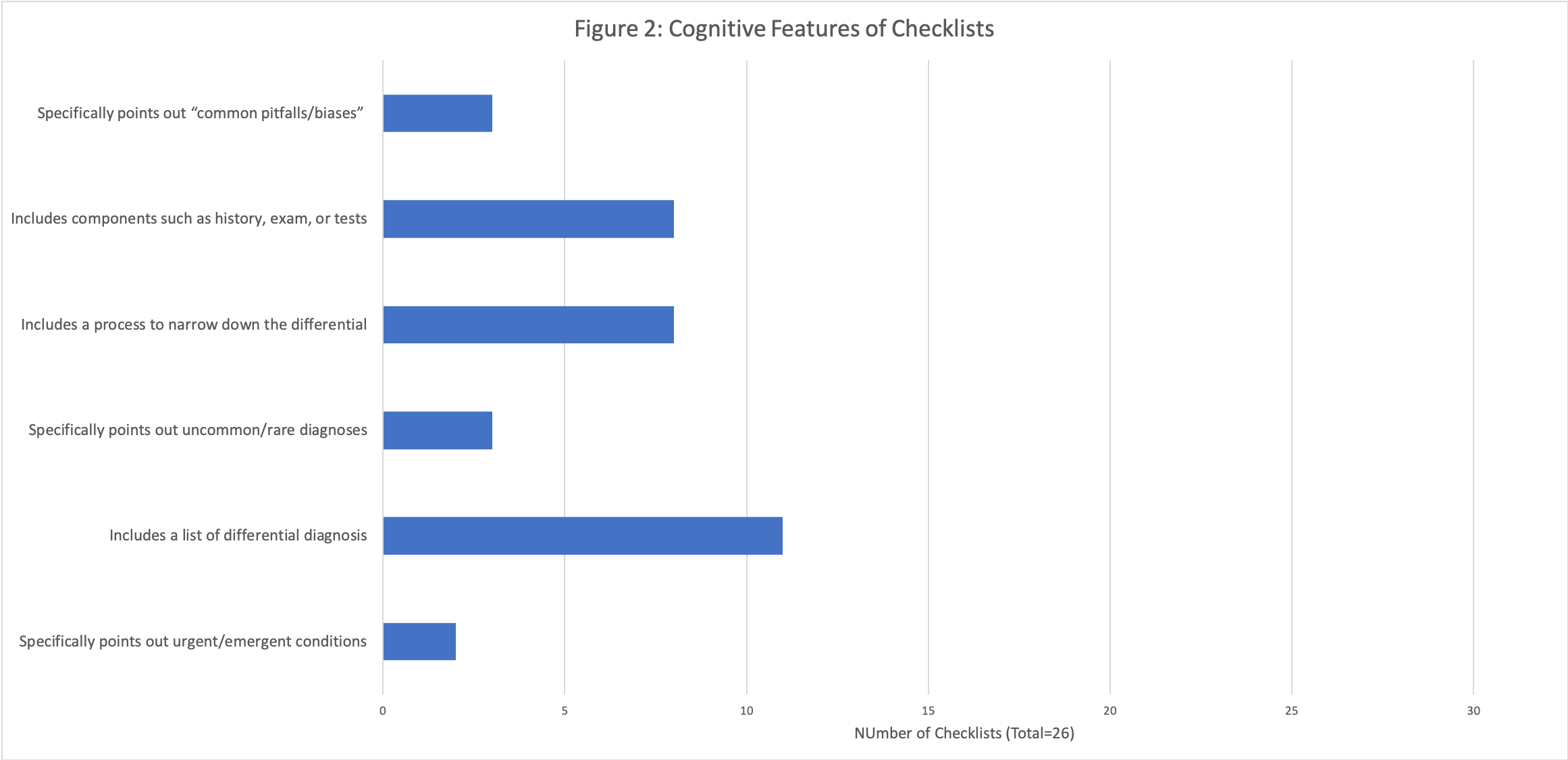
Results: The search resulted in a total of 4,812 citations. After title and abstract screening, 53 studies underwent full text review and 23 studies were included. Of the 23 included studies, five were randomized controlled trials, and 18 were observational, quasi-experimental (e.g. pre-post), or checklist proposal studies. A total of 23 distinct checklists were retrieved from the 23 studies. Five studies included more than one checklist, while 9 studies included checklists already published in one of the other included articles. Included checklists focused on the following SEIPS categories (Figure 1): cognitive processes (23 checklists), persons (9), patient outcomes (7), tasks (6), internal environment (3), physical processes (2), and social and behavioral process (1). Of note, no checklists focused on SEIPS categories such as tools and technologies, external environment, or professional and organizational outcomes. With respect to cognitive components, 11 checklists included a list of differential diagnosis, 8 included a process to help narrow down the differential, 8 included components such as physical exam or tests, 3 included a list of common pitfalls or biases, 3 highlighted rare medical conditions, and 2 highlighted urgent medical conditions (Figure 2).
Conclusions: In this systematic review of 23 studies and 23 diagnostic checklists, considerable variation in checklist content was observed. Most checklists emphasized cognitive elements, while some focused on patient outcomes. Few focused on work system elements such as tasks, persons, organization, and internal environment. No checklists focused on other elements such as tools and technologies or external environment. Furthermore, less than a quarter of the checklists focused on potentially important cognitive diagnostic features such as highlighting urgent or rare medical conditions, or common diagnostic pitfalls. Because diagnosis is the product of physicians working within work environments, better integration of human factors in checklist design and diagnosis appears necessary.