Background:
The transition of care between providers constitutes a vulnerable point in the care of a hospitalized patient. Poor‐quality or inadequate handoffs have been identified as a nidus for adverse clinical events. As shift restrictions have necessitated change in the practice of medicine, there are a greater number of inpatient handoffs in a single day. It has been suggested that handoffs improve patient safety during transitions of care. Thus, standardizing inpatient handoffs may mean fewer adverse events for the hospitalized patient. Several studies examined the handoff process, but few offered quantifiable data to reflect the influence that the handoff process has on patient outcomes. This study compared the frequency of adverse clinical events between patients admitted with and without a standardized handoff of care between admitting providers and the hospitalist team caring for the patient.
Methods:
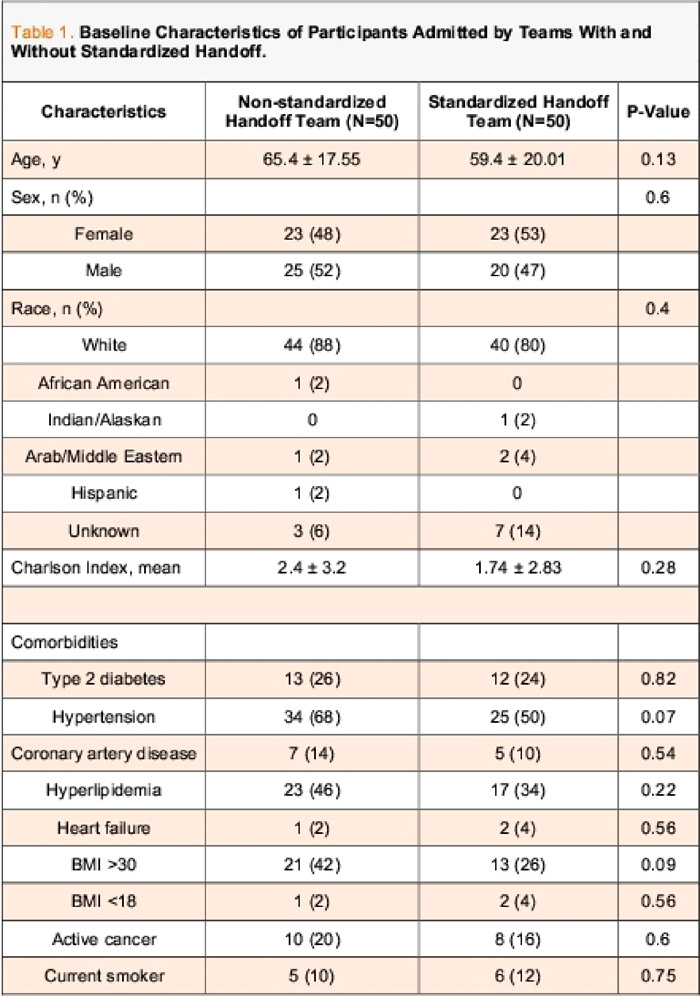
We conducted a retrospective study of the first 100 patients admitted to hospitalist teams by hospitalist admitters with and without standardized handoffs of care at Mayo Clinic in August 2011 (Table 1). We defined the frequency of mortality, rapid response/code blue, transfer to higher acuity care, and events identified by the Global Trigger Tool as primary outcomes. We compared these variables between patients admitted to teams with and without a standardized handoff. Secondary outcomes included the 30‐day readmission rate and length of stay, which were compared between the 2 groups. Statistical analysis of primary and secondary outcomes used Fischer's exact test for categorical variables and the Student t test for continuous variables. Global Trigger Tool data were analyzed using a negative binomial regression model.
Results:
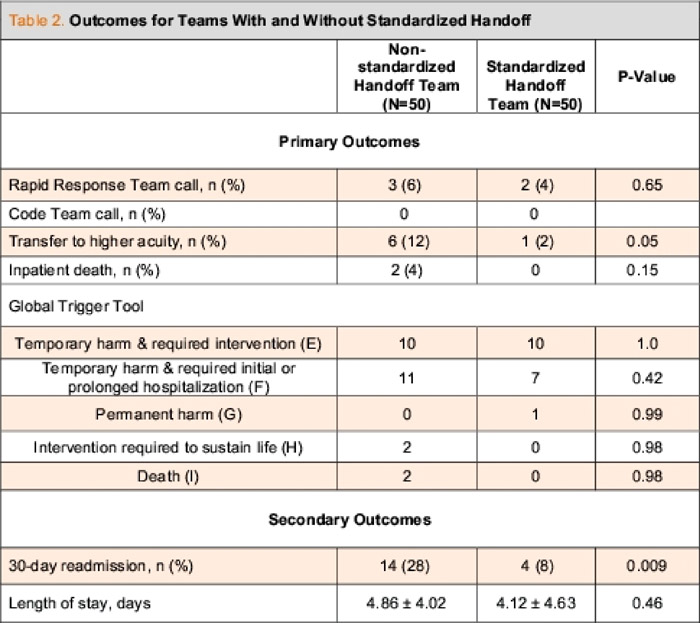
There was no statistically significant difference in the frequency of the primary outcomes in patients admitted by teams with and without standardized handoffs (Table 2). The secondary outcome of 30‐day readmission rate was higher for those patients admitted by the nonstandardized handoff team (P = 0.009).
Conclusions:
There was no difference in the primary outcomes between patients admitted to teams with and without standardized handoffs. However, patients admitted by the nonstandardized handoff team had a higher rate of 30‐day readmission compared with those patients admitted by the standardized handoff team. Rate of transfer to higher acuity care was greater among patients admitted by the nonstandardized handoff team and approached statistical significance (P = 0.05). Patients admitted without a standardized handoff between admitters and hospitalist teams were no more likely to experience an adverse clinical event than those patients admitted with a standardized handoff.