Background: Hospital medicine is one of the fastest growing specialties in the United States (1). As more residency graduates pursue careers in hospital medicine, growth of dedicated post-graduate hospitalist fellowship programs has also occurred. These fellowship programs are intended to prepare participants for careers in academic hospital medicine as career paths within hospital medicine vary widely (2). There is limited data surrounding specific fellowship experiences (3). Using data from a large academic center with a well-established hospitalist fellowship program, we aimed to quantify how clinical experiences of hospitalist fellows vary across years.
Methods: Established in 2005, the Hospitalist Scholars Training Program at the University of Chicago offers a flexible fellowship program of 1-3 years with 1-5 fellows a year. Using clinical scheduling data from an internal web-based scheduler from May 2013 to June 2020, we characterized clinical shifts as day service, off-hour service, teaching service, consult service, or jeopardy. Day service consists of 10-hour traditional inpatient care shifts. Off-hour service includes 8 or 12-hour evening/night admitting and cross-coverage shifts. On the teaching service, fellows supervise general medicine housestaff teams. Consult service comprises general medicine consultation with trainees rotating 60% of the time. Jeopardy involves back-up call shifts activated to cover high patient census or sick coverage.
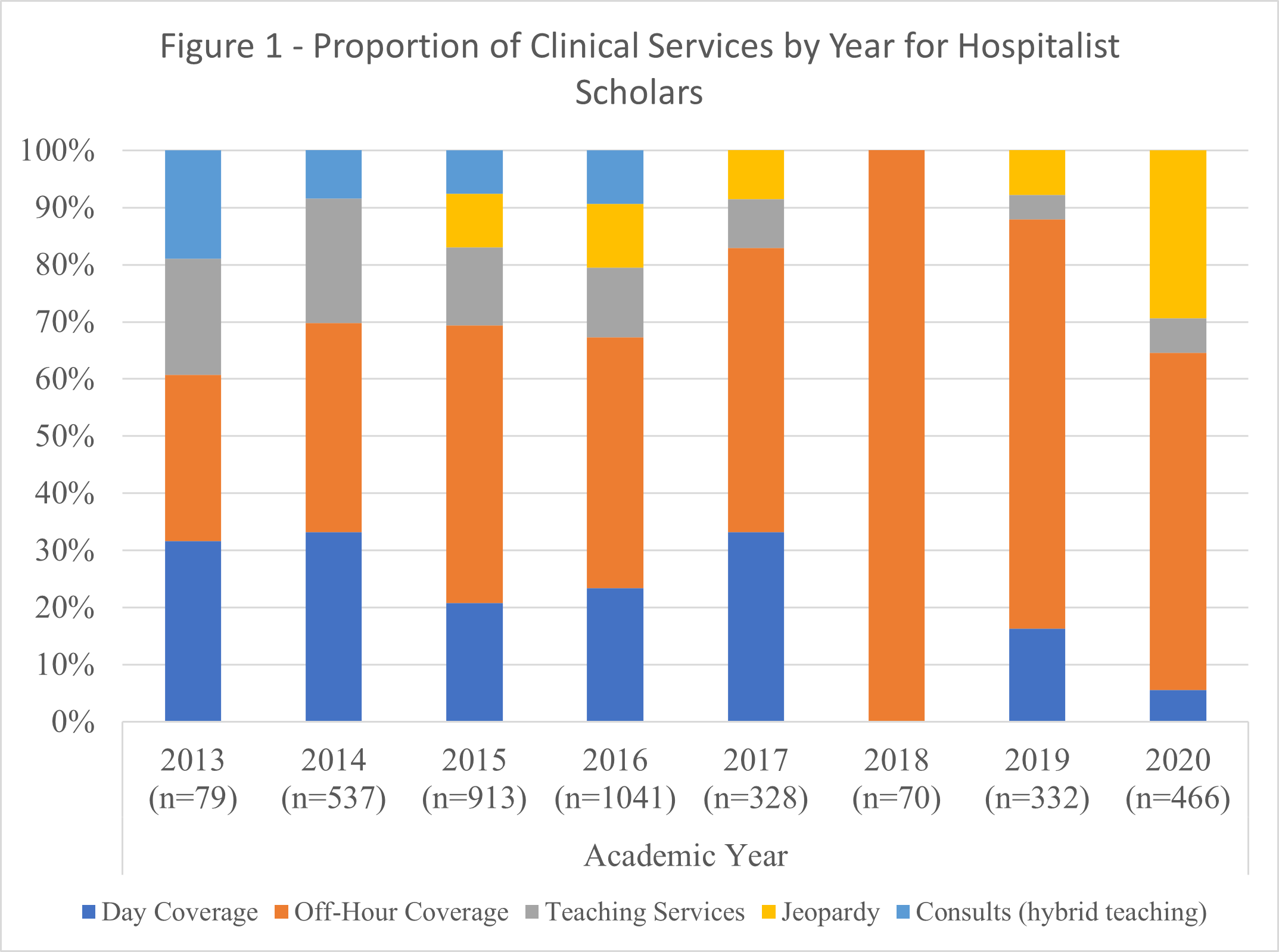
Results: Across 7 years of data, there were 23 fellows, and 3,766 clinical service shifts logged. The mean number of shifts per provider during fellowship was 164, increasing to 195 when removing data from providers who only had shifts in 2013 or 2020. Figure 1 shows distribution of clinical service types over time. Off-hour and day service accounted for more than 60% of shifts completed by fellows. Off-hour service has increased over the last two years, with corresponding decreases in day service, 21-33% in 2013-2017 to 6-16%, and teaching service, 14-22% in 2013-2014 to 4-6%, in the last two years. Similarly, participation in consult service decreased.
Conclusions: Our snapshot of the breakdown of clinical duties assigned to hospitalist fellows at one large major academic hospital reveals relatively stable numbers of shifts worked over time, but considerable variability and large swings in the types of shifts completed. Day service and teaching service participation has decreased while off-service shifts have become more common for fellows, ranging from 50-100% of shifts from 2017-2020. Off-hours shifts afford more flexibility in scheduling, but dominance in off-hours shifts may not be adequate preparation for a career in academic hospital medicine. The clinical composition of academic hospitalist careers has not been well-described, and is an important area for future study. There is currently no guidance for clinical exposure for hospitalist fellows during training fellowship programs. There is likely considerable heterogeneity in the clinical exposure hospitalist fellows experience across the country. Further study is necessary to understand how clinical experiences affect development and to improve standardization of clinical and non-clinical endeavors for fellows in adult hospital medicine. Our results are limited to one institution and may not generalize to experiences at other programs, but represent the first description to our knowledge of the clinical experiences of an adult hospital medicine fellowship program.