Background:
Cardiopulmonary resuscitation (CPR) is part of the standard of care for the event of cardiac arrest during hospital admissions. The “do not resuscitate” (DNR) order documents that patients do not wish to pursue CPR in the event of cardiopulmonary arrest (CPA). The Ministry of Health has announced that 69.7% of middle-aged home residents in Japan agree with writing advance directives, but only 3.2% of them actually had prepared it. In that survey, 68.8% of people would like DNR in case of end stage of cancer. However, there has been no report which investigates the in-patients’ preference regarding code status. We investigated it.
Methods:
We conducted cross-sectional survey by chart review.
All acute care patients, who admitted to general ward of internal medicine in our hospital from January 29th to February 28thin 2015 were included. We obtained the age, gender, the place of living (home or long term care facility), ability of ADLs and IADLs, to evaluate their association with DNR status by multivariate analysis. We also assessed patient’s decision-making capacity on admission. Decision making capacity is classified into “completely capable”, “partially capable”, and “not capable at all”. Their request of code status is classified into full code and Do-Not-Resuscitate (DNR).
Results:
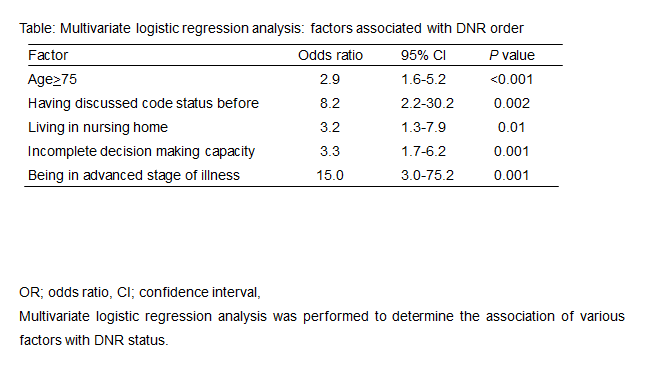
527 patients met the criteria. 194 were excluded due to lack of data and 333 were analyzable (63%). The age was 75(median, 62-84). 179 (53.8%) were male.113 (33.3%) requested for DNR in case of CPA. 170 (51%) were 75 years old (yo) and older. 43 (12.9%) were living in nursing home. 97 (29.1%) do not have complete decision making capacity. The age of 75 yo and older, experience of discussing the code status with physicians in the past, being nursing home resident, incomplete decision making capacity and being in advanced stage of illness were associated with requesting for DNR by multivariate logistic regression analysis (as shown in table).
Conclusions:
DNR was requested by 33.3% of patients on admission. The associated factor were age≧75, experience of discussing the code status in the past, nursing home resident, and incomplete decision making capacity. Before losing decision-making capacity, we need to consider discussing code status preference with patients.