Background: Understanding a patient’s goals of care (GOC) during hospitalization is vital to provide patient centered care. Despite the known importance, little is known about the quality of GOC conversation documentation. The aim of this study is to examine discussion documentation in hospitalized general medicine (GM) patients prior to intensive care unit (ICU) transfer and factors associated with documentation quality.
Methods: Patients > 18 years old admitted to GM at an academic medical center with subsequent rapid response team (RRT) activation and transfer to the ICU from 7/2022 – 6/2024 were identified. Patients were excluded if admitted directly to an ICU or if RRT < 24 hours after admission. Variables collected included demographic features, Charlson comorbidity index (CCI) score, team structure (faculty vs resident), length of stay (LOS) prior to ICU transfer, code status order, and palliative care consultation. Quality of GOC documentation was assessed based on presence of five key components previously described in the literature: mention of prognosis or patient understanding of illness, patient values and/or goals, identification of durable power of attorney (DPOA) or personal representative, use of and/or limitations of specific life sustaining interventions, and participants in discussion. Documentation of >= 2 components – excluding mention of participants – was considered high quality GOC documentation. Data was analyzed using bivariate analysis and logistic regression models.
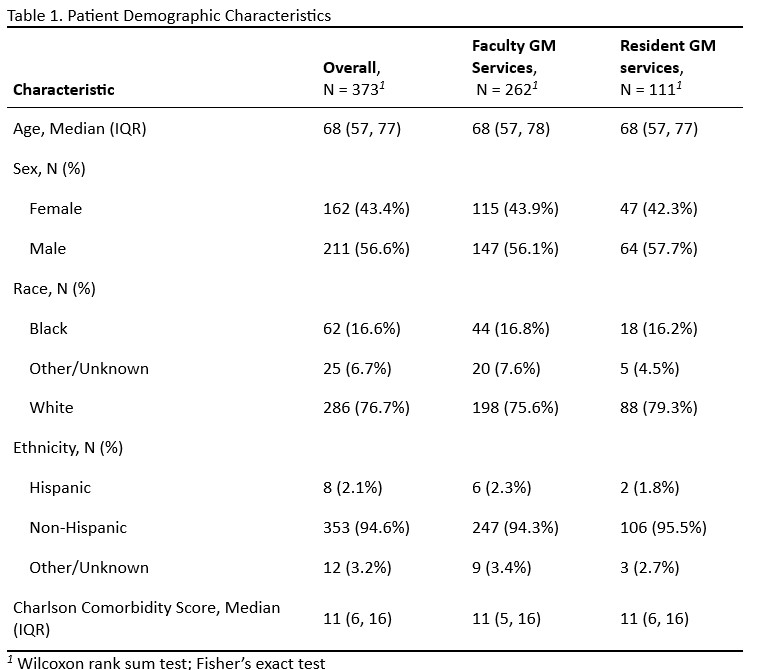
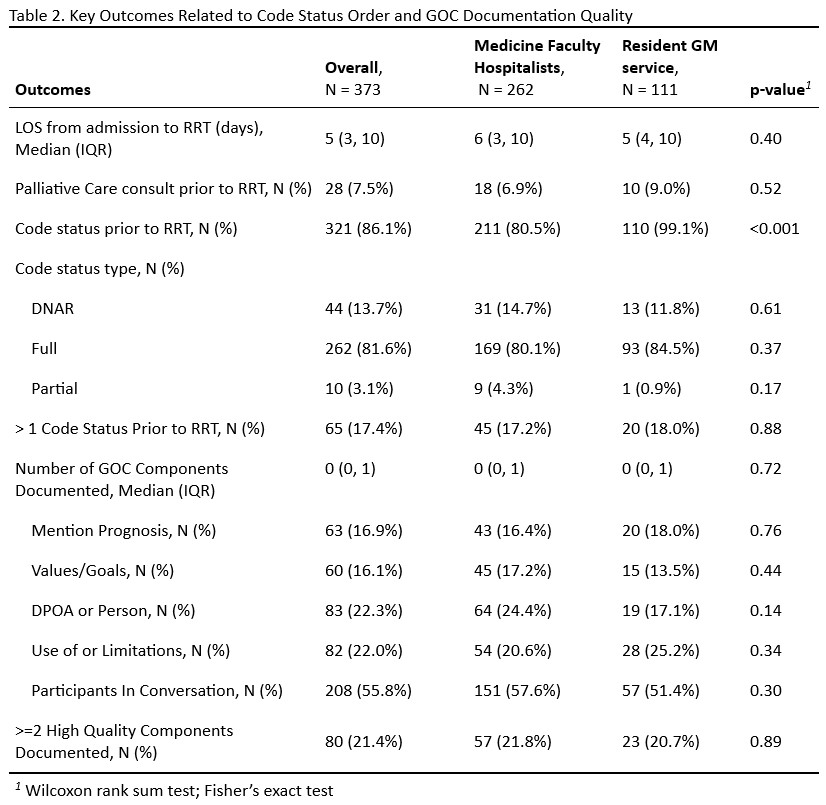
Results: A total of 373 patients met inclusion criteria for analysis with 70% admitted to a faculty service and 30% to resident services. Table 1 describes demographic characteristics of the sample. 19% of patients required intubation within 24 hours of ICU transfer, 45% vasopressors, and 39% died during hospitalization. Table 2 describes code status order frequency and quality of GOC documentation. The majority of patients (86.1%) had a code status order prior to ICU transfer; patients on faculty compared to resident services were less likely to have an order (80.5% vs 99.5%, p < 0.001). Nearly 40% of patients had no components of GOC conversations documented; the most frequently documented was who participated (55.8% of encounters). Few patients (21.4%) had >= 2 high quality GOC components documented. Factors associated with higher quality documentation in multivariable logistic regression included older age (IRR 1.03, 95% CI 1.02-1.04), higher CCI score (IRR 1.03, 95% CI 1.0-1.05), and longer LOS prior to RRT (IRR 1.04, 95% CI 1.02-1.06).
Conclusions: Our data suggests that physicians are infrequently documenting key components of high quality GOC conversations in ill hospitalized adults prior to ICU transfer. Older patients with multiple comorbidities and those with longer pre-ICU hospital LOS were more likely to have higher quality documentation. More work is needed to understand reasons for low quality documentation and impact on patient care and outcomes.