Background: Clostridium difficile infections (CDI) is a notorious nosocomial threat to health and a leading cause of infectious diarrhea. It is associated with billions of dollars of US health care costs annually due to long hospital stays and readmissions. While CDI is mostly caused by toxin-producing strains, some strains do not express these proteins. These non-toxigenic strains C. difficile (NTCD) have drawn attention for their capacity to colonize humans and potentially reduce the risk of symptomatic CDI caused by the toxigenic strains. This meta-analysis is performed to evaluate the evidence supporting colonization with NTCD, either naturally acquired or induced by using oral forms, can lower subsequent CDI.
Methods: We searched the PubMed database using the term “nontoxigenic Clostridium difficile”. Additional manuscripts were identified by reviewing the bibliographies of published articles. We selected all cohort and randomized studies where patients colonized with NTCD was compared with those without NTCD and reported on the development of primary CDI or recurrent diarrhea. We calculated the pooled relative risk (RR) with the corresponding 95% confidence interval (CI) for the development of recurrent CDI or development of diarrhea by using the fixed effects method
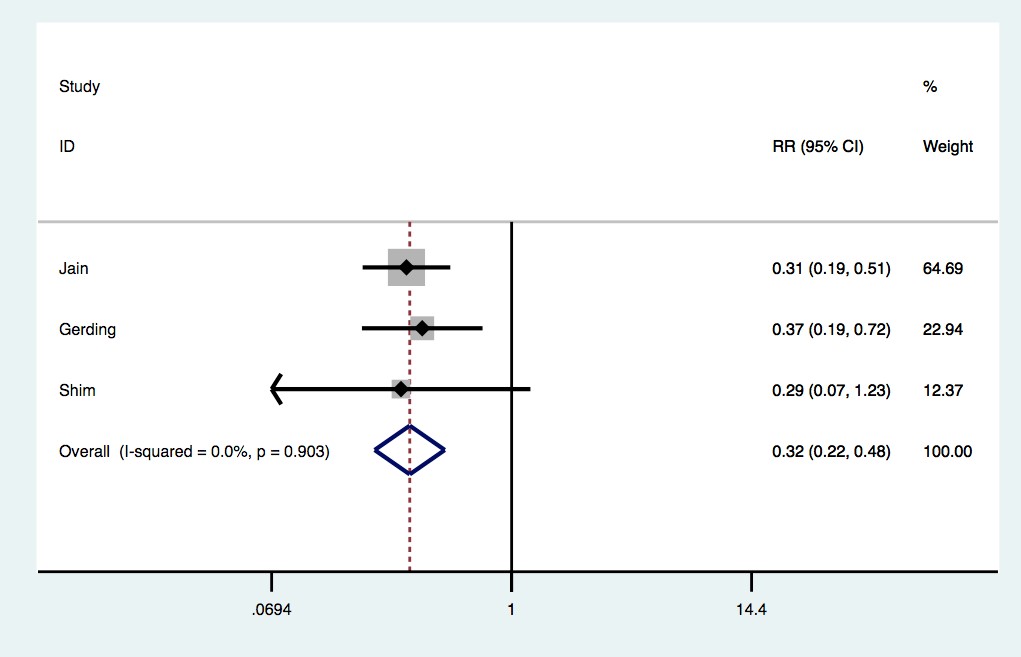
Results: The search strategy yielded six studies, of which only 3 met our eligibility criteria. The studies comprised 1,128 evaluable patients with a median age of 54 and 48% females ,and included 12% with prior CDI, 58% with antibiotic use and 41% with proton pump inhibitor use. The pooled relative risk of having CDI or recurrence for those colonized with NTCD or given oral forms is 0.32 (95% CI 0.28-0.47, p<0.01) compared to those not colonized or receiving placebo.
Conclusions: NTCD colonization appears to be associated with a lower risk of subsequent CDI. With respect to using NTCD as a therapeutic, intentional colonization is found to be protective. The potential use of an oral NTCD as a ‘probiotic’ would be a major milestone in preventing CDI and its recurrences. It will not only keep patients safe and avoid unnecessary costs, but also will provide an easier and more palatable option compared to other treatment options such as fecal transplant.