Background: The rate of burnout among health care providers is unacceptably high and recent scholarship has advocated for organization-facing interventions to tackle this problem. To that end, our large academic hospital medicine group has developed a multi-modal strategy to identify high-yield interventions for provider well-being. A part of this initiative involved piloting a digital survey tool with the goal of monitoring hospitalists’ experience of clinical work and prioritizing improvement opportunities.
Purpose: We utilized a novel (Waggl) software platform to develop a “Clinician Voice” pulse survey in order to garner hospitalist engagement around their clinical work experience and prioritize improvement opportunities.
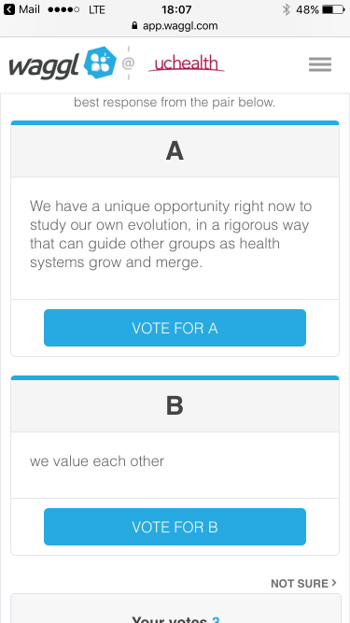
Description: The Waggl platform offers unique features compared to traditional engagement surveying methodologies. For one, survey length on the platform is limited to 5 quantitative questions and 1 qualitative question. In addition, Waggl includes an interactive component whereby participants prioritize their own qualitative answer as compared to answers entered by their colleagues in an A-B voting format (Figure 1.). Over time, this creates a “crowdsourced” priority list related to qualitative responses. Prior to our pilot, we consulted key hospital stakeholders, including the Chief Medical Officer, and committed to an overall engagement process to follow up the survey with an inclusive dialog of the results. Over 7 days, all physicians and advanced practice hospitalists in our group were invited to participate in a two question survey using their browser or mobile device. The first question asked participants to rate the likelihood that they would recommend their clinical workplace to a friend on a quantitative 0-10 scale. The second question asked “What would make it more likely for you to give a 10 rating on the first question?” 24 hospitalists (34%) participated in the survey and cast 147 priority votes. An in-person dialog was held at a subsequent hospitalist faculty meeting to review the survey process and better understand the factors contributing to the priorities that emerged from the survey. Outputs from the survey and dialog were shared with hospital executives to inform decision making and used by hospitalist leadership for strategic planning. As a result of the pilot, the process was adopted across several other clinical specialties.
Conclusions: Interactive digital survey instruments can be leveraged to assess frontline work experience, create productive dialogue between frontline clinicians and leaders, and identify improvement opportunities.