Background: Strong evidence exists showing that effective communication in healthcare conversations improves outcomes such as patient satisfaction, safety, reduced malpractice suits, physician professional fulfillment and burnout prevention. Formal communication skills training in medical education is often limited to targeted sessions such as those focused on delivering bad news, code status and end of life care decisions. These programs often pre-suppose a basic competency in foundational skills which may not be present, thereby limiting their effectiveness.
Purpose: Develop and pilot a communication skills training course for internal medicine residents relevant to caring for inpatients on the internal medicine service using active learning strategies such as role playing, simulation, and focused reflection.
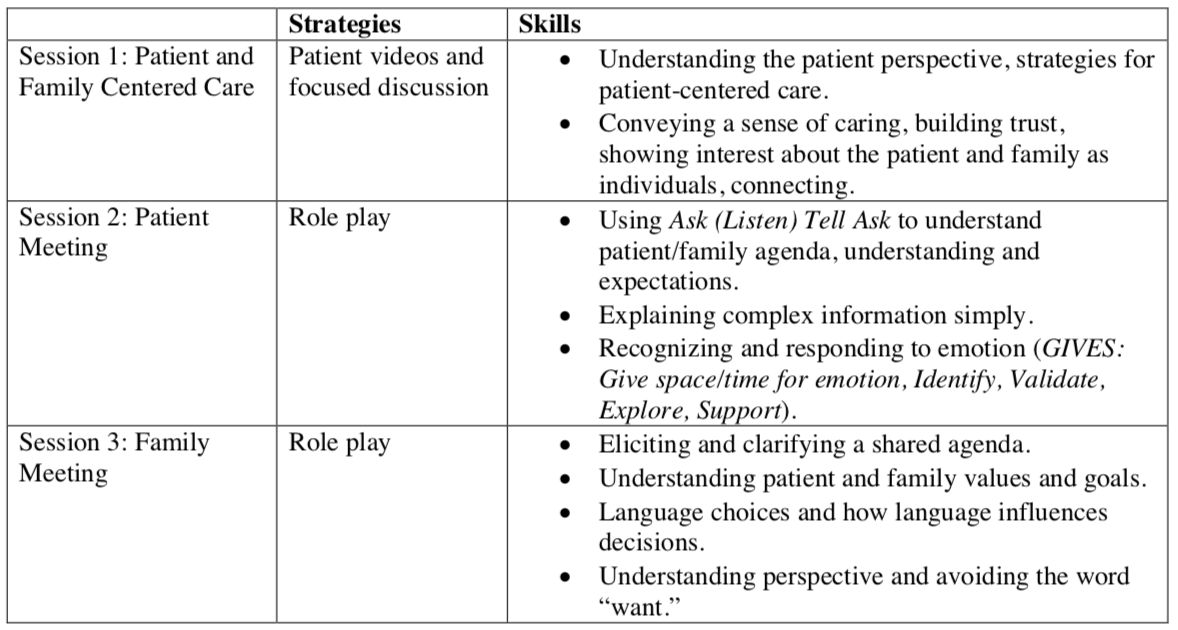
Description: We developed and delivered a communication course to all PGY1 internal medicine residents at our academic center. The curriculum was developed in collaboration with faculty at Beth Israel Deaconess Medical Center and based on an existing course there for residents rotating in the ICU. Materials were delivered in small groups over three sessions for a total of 3 hours of didactic time. All sessions were led by faculty in the Division of Hospital Medicine. Hospitalists care for all medicine inpatients at our academic center. We developed a Communication Guide describing key skills and phrases for effective communication, which was incorporated in the teaching sessions. Topics covered during each session and educational methods are outlined in the table below. Throughout the curriculum, residents reflected on patient interactions in which they perceived difficult or poor communication. Focused feedback was provided by residents and faculty. Residents were asked to self-evaluate their skills with a pre-course survey, post-course survey and a 3-month follow up survey. Fifty percent of residents had not received any formal communication training prior to residency, yet every resident had been responsible for leading family meetings that year. Following the course, residents felt they had improved in leading a family meeting, setting the meeting agenda, delivering bad or distressing news, discussing code status, next steps, psychosocial needs, and the transition to palliative care, dealing with conflict among family members, verbally and non-verbally expressing empathy, and letting patients and families know their concerns are understood. These improvements were sustained over a 3-month period. Sixty-five percent of residents reported that they had changed at least one communication practice after taking the course with responses such as:“Wait longer for responses (allow for silence)”
“Address emotions more directly”
“Establish what the family does/does not know”
“Attempt to listen to patients’ feelings and validate/reassure rather than just talk medical jargon”
Conclusions: Many internal medicine interns do not receive formal communication training prior to internship and those who do often receive situation-specific training. A brief program using learning techniques for teaching core communication tools to all interns is feasible and can improve self-perceived communication skills across many domains.