Background: The placement of peripherally inserted central catheters (PICCs) is increasingly performed primarily by vascular access nurses (VAN) in United States hospitals1. Despite the increased use of these specially trained clinicians, little is known about the patient and device characteristics of the PICCs they placed compared to those placed by interventional radiology (IR) providers. While there is some evidence that VAN device placements are associated with low device-related complication rates, comparison to IR specialists cannot be made without accounting for likely differences in patient and device selection. In this study, we describe the patient and device characteristics of PICC placements by these two groups.
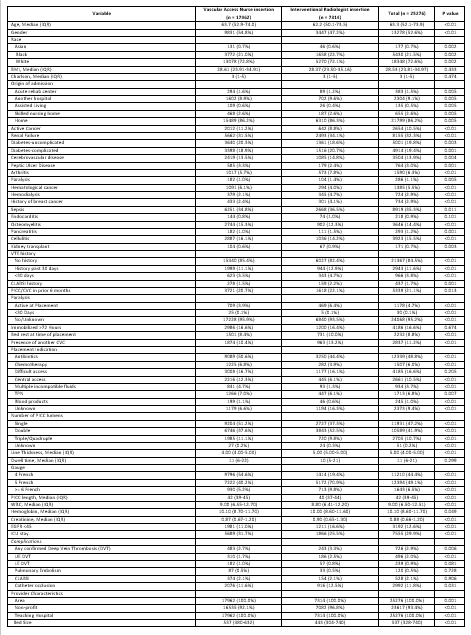
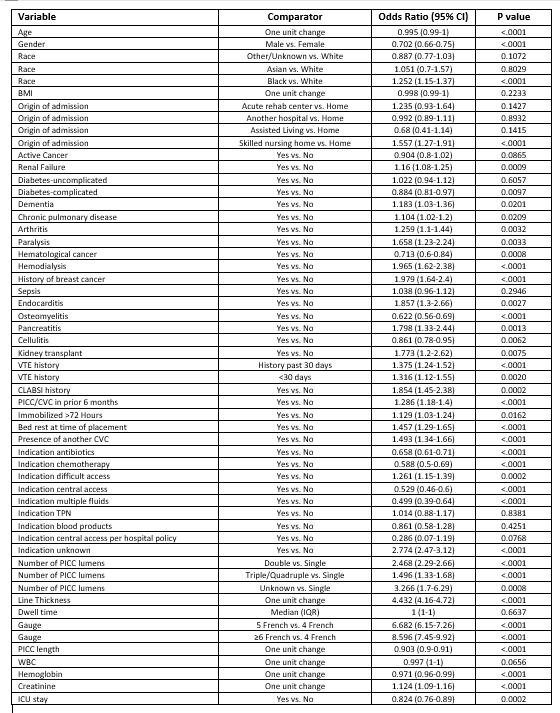
Methods: From January 2013 to November 2022, trained abstractors collected demographic and clinical data on patients receiving PICCs while hospitalized at 13 hospitals participating in the Michigan Hospital Medicine Safety Consortium. At these hospitals PICCs are routinely placed by both VAN and IR providers. PICC placements by VAN were compared to those placed by IR based on patient and device characteristics. Device selection measures included preference for single-lumen devices, avoidance of short dwell times (less than 5 days), and avoidance of PICCs in patients with eGFR < 45 ml/min/1.73m2. Patients were followed until PICC removal, for 30 days following PICC placement or death, whichever occurred first. Chi-square tests were used to compare categorical variables and t-tests and Wilcoxon rank-sum tests for continuous variables. Associations between patient characteristics and placements by VAN or IR were also estimated using mixed-effects logistic regression models, accounting for hospital-level clustering.
Results: A total of 25,276 PICCs placed were included in the analysis. Of these, 17,963 (71.1%) were placed by VAN and 7,314 (28.9%) by IR. Patient characteristics varied greatly across provider types. Compared to PICCs placed by VAN, those placed by IR were more likely in patients with renal failure (34.1% vs. 31.5%; p< 0.01), paralysis (6.4% vs. 3.9%; p< 0.01), a history of breast cancer (4.1% vs. 2.4%; p< 0.01) and another central venous catheter already in place (13.2% vs. 10.4%; p< 0.01). IR-placed PICCs were less likely to be single-lumen devices (37.3% vs. 51.2%; p< 0.01), were more frequently removed within 5 days (21.2% vs. 17.0%; p< 0.01) and had a higher proportion of patients with eGFR < 45 ml/min/1.73m2 (16.6% vs. 11.0%; p< 0.01).
Conclusions: We found significant differences in patient and device characteristics when comparing vascular access nurse and interventional radiologist PICC placements. Because of these differences in patient and device selection and their established correlation with PICC-related outcomes, methods such as target-trial emulation are needed to evaluate the true association between catheter outcomes and these two provider types.