Background: Previous research indicates that delayed transfer of patients to critical care units from Medical-Surgical units results in increased mortality. However, few studies have compared the outcomes of patients directly admitted from the emergency department (ED) to the intermediate care units (IMC) to those of patients admitted to Medical-Surgical (floor bed) status and subsequently transferred to IMC.
Methods: We investigated the demographics, clinical features, and hospital length of stay of 10,316 patients transferred within 6 or 24 hours vs. directly admitted to the IMC.
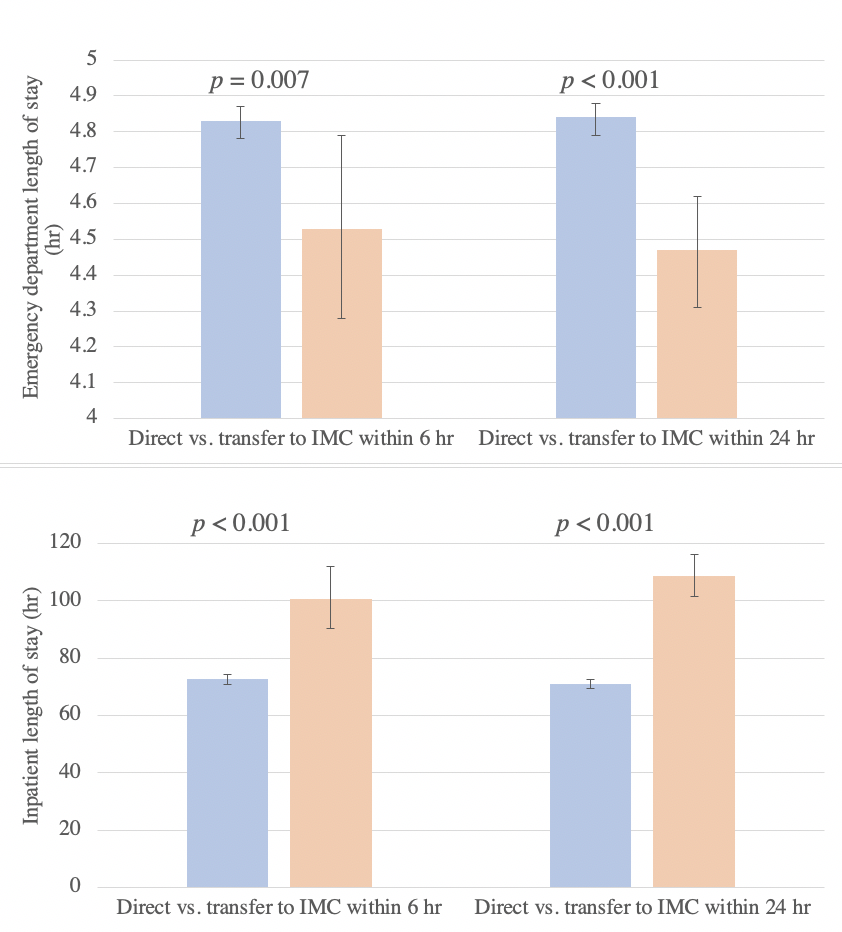
Results: As opposed to patients directly admitted to the IMC, significant increases in inpatient LOS were noted in patients transferred to IMC from Medical-Surgical status in 6 hours or less (137.90 vs 100.91 hr) and in 24 hours or less (141.95 vs 98.04 hr) (p<0.01), despite the fact that patients directly admitted to the IMC were more likely to be of higher acuity (defined as Emergency Severity Index [ESI] score of 1 or 2; 49.70% vs 39.20% at 6 hours, 49.40% vs 35.00% at 24 hours, p<0.01). Similar results were found in a linear regression model to determine LOS that controlled for age and ESI (Figure 1).
Conclusions: Patients admitted to Medical-Surgical status who are transferred to an intermediate unit have a longer hospital LOS than those who were admitted directly to an IMC unit, despite the fact that they were of lower initial acuity. These results suggest that, when deciding between Medical-Surgical and IMC status, inpatient length of stay is correlated with accurate initial status.