Background: Hospital discharge is a complex and dangerous process. The emergence and rapid growth of the Hospitalist specialty with the simultaneous decline of traditional practice models complicates discharges. In light of the discontinuity, it is crucial to build reliable communication tools that facilitate transmission of critical information.The discharge summary is an essential piece of that transition and is often the only means of communication between the hospital and the outpatient provider. A well written, thorough, accurate, and timely discharge summary may help to prevent 30-day hospital re-admissions. Although the Joint Commission and the Center for Medicare and Medicaid Services both published guidelines for the structure of discharge summaries, it is unclear how outpatient providers use this information. In addition, formal training surrounding discharge summaries within residency programs has traditionally been lacking. Many studies demonstrate frequent inaccuracies or missing components from discharge summaries 一 they often lack information that outpatient providers may find most useful, e.g. reasoning behind medication changes, and are not completed prior to the post-hospital visit.
Purpose: To further delineate the most useful elements of discharge summaries, we conducted a multi-center, multi-specialty survey of Internal Medicine, Family Practice, and Pediatric practitioners that assessed providers’ preferences and how they utilized these resources.
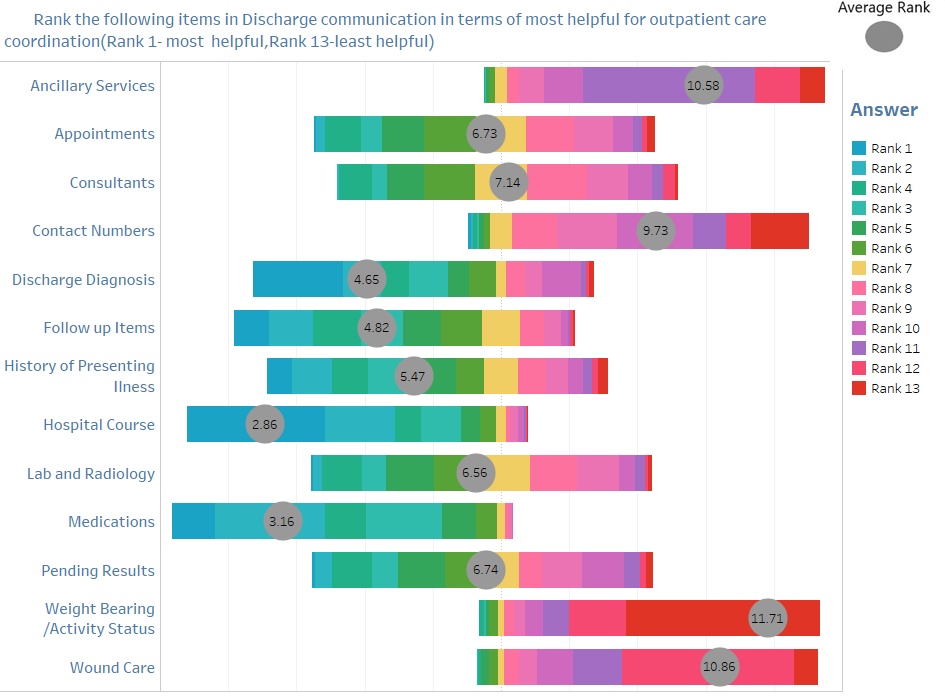
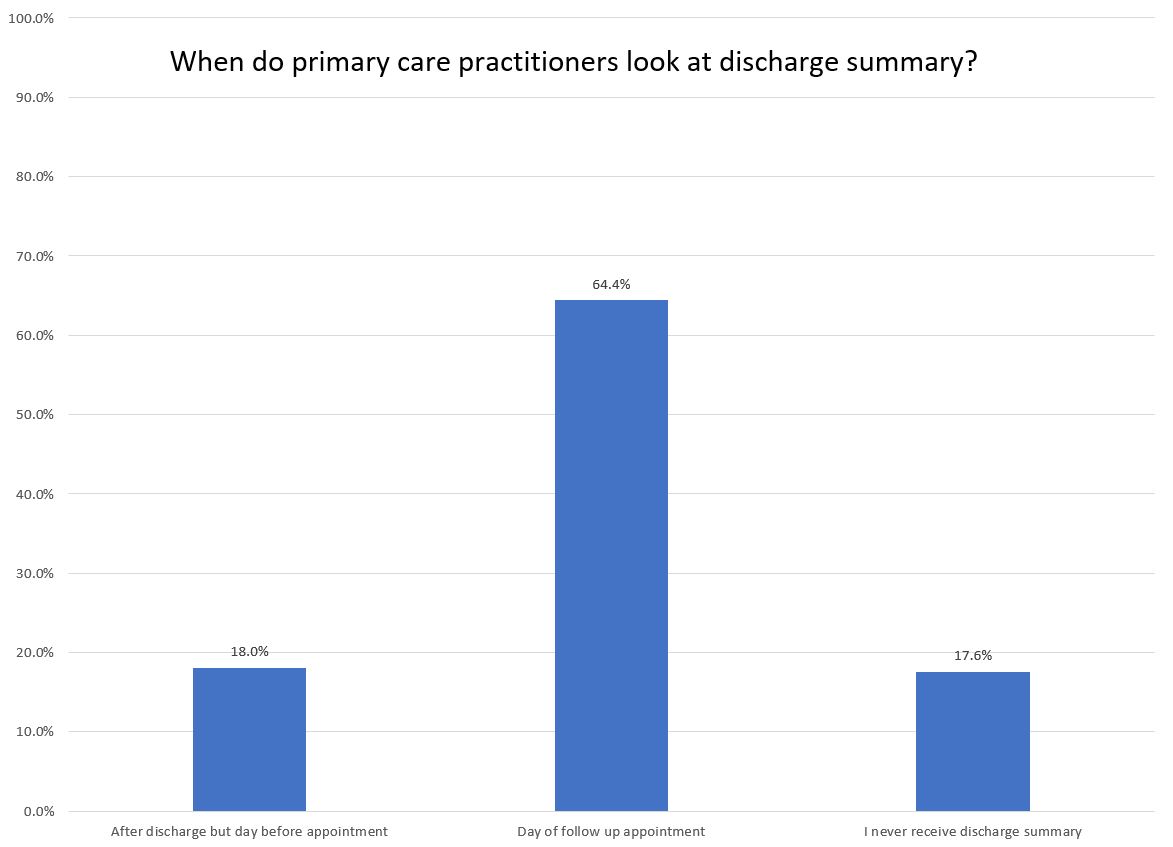
Description: Outpatient providers considered 一 in descending order 一 the hospital course, medications, discharge diagnoses, follow-up instructions, and HPI to be the most important components of discharge summaries. Labs and radiology were less important while weight bearing status, wound care, ancillary services, and consults were ranked lowest. Most outpatient providers read the summary the day of the appointment and 60% of respondents said it was the only source of communication with inpatient providers.
Conclusions: Using this information, it is feasible to create a standardized template that will increase efficiency of both hospitalists and outpatient providers and help to safely transition care. The most crucial elements that should be prioritized at the beginning of the summary are hospital course, complete medication list, discharge diagnoses, and history of present illness. Based on this large data set, we strongly believe that the creation of a standardized discharge summary template will lead to a more efficient and effective discharge process, with fewer re-admissions and safer transition out of the hospital.